Simplified in Practice: ECG nuggets for atrial fibrillation
M3 India Newsdesk Nov 04, 2021
The most frequent kind of arrhythmia is atrial fibrillation, which occurs when the heartbeat is irregular. In this segment of our series of Simplified in Practice, we bring to you the common ECG features of AF along with practice pointers for management.
When atrial electrical activity and contraction are disorganised, it is a sign of it. AF is becoming more common and prevalent. Lifetime risk falls below 25% at the age of 40. Haemodynamic instability, cardiomyopathy, heart failure, and embolic events such as stroke are all possible side effects of AF.
Atrial fibrillation electrocardiogram (ECG) characteristics
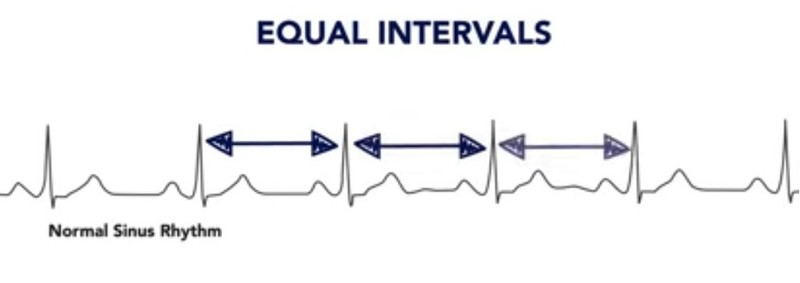
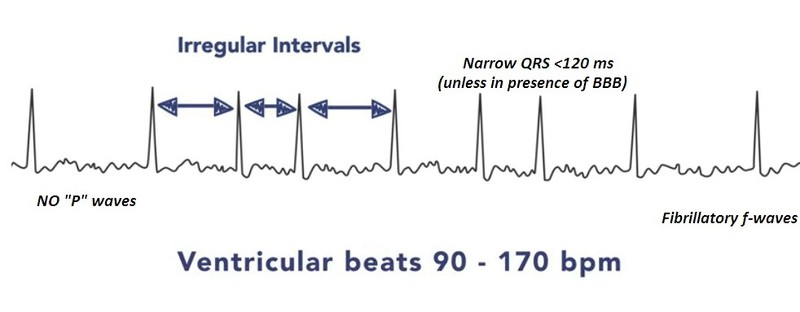
- A beat that is irregularly erratic.
- There are no P waves.
- There is no isoelectric baseline.
- Variable ventricular rate.
- QRS complexes are typically fewer than 120 ms unless there is a pre-existing bundle branch block, auxiliary route, or rate-related conduction abnormality.
- Fibrillatory waves may be present and might be small (amplitude less than or equal to 0.5mm) or coarse (amplitude more than 0.5mm).
- Fibrillatory waves might be mistaken for P waves, resulting in a misdiagnosis.
ECG in AF
How does atrial fibrillation occur?
Although the processes behind AF remain unknown, it needs a starting event (focal atrial activity/PACs) and a substrate for maintenance (i.e. dilated left atrium). The following processes have been proposed:
- Focused activation - Here AF comes from a focal region of activity. This activity may be induced as a result of greater automation or as a result of micro-reentry. It is frequently found in pulmonary veins.
- Multiple wavelet mechanism- In this technique a large number of little wandering wavelets are generated. The fibrillation is sustained via re-entry circuits produced by many wavelets. This process is accelerated when the LA is dilated. The increased surface area enables continuous waveform propagation.
Causes of atrial fibrillation
- Hypertension
- Ischaemic heart disease
- Valvular heart disease (especially mitral stenosis/regurgitation)
- Electrolyte disturbance (hypokalaemia, hypomagnesaemia)
- Acute infections
- Thyrotoxicosis
- Drugs (e.g. sympathomimetics)
- Alcohol
- Pericardial disease
- Pulmonary embolus
- Acid-base disturbance
- Pre-excitation syndromes
- Cardiomyopathies: dilated, hypertrophic
- Phaeochromocytoma
Additional characteristics of AF
- Ashman phenomenon - atypical ventricular conducted beats, often of the RBBB type, caused by a prolonged refractory time as indicated by the previous R-R interval.
- In AF, the ventricular response and hence the ventricular rate are determined by a number of variables, including vagal tone, additional pacemaker foci, AV node function, refractory time, and medicines.
- AF is most often linked with a ventricular rhythm of 110–160 beats per minute.
- When the ventricular rate exceeds 100 beats per minute, AF is often characterised as having a 'rapid ventricular response.'
- 'Slow' AF is a phrase that is often used to refer to AF with a ventricular rate of fewer than 60 beats per minute.
- Hypothermia, digoxin toxicity, medicines, and sinus node dysfunction are all possible causes of slow AF.
AF classification
The classification is based on the presentation and duration of atrial fibrillation as follows:
- The first episode - regardless of symptoms or length, the initial discovery of AF
- Recurrent AF - More than two occurrences of AF in a 12-month period.
- Paroxysmal AF - <7-day self-terminating episode
- Persistent AF - AF that does not self-terminate, duration more than 7 days
- Persistent AF - over an extended period of time – >1 year
- Indefinite (Accepted) AF - A period of more than one year during which rhythm control treatments are not attempted or are ineffective
Important - Paroxysmal AF lasting more than 48 hours is unlikely to spontaneously convert to sinus rhythm, and anticoagulation should be proposed.
Atrial fibrillation treatment
Atrial fibrillation management is complicated and is dependent on the duration of the condition, co-morbidities, underlying aetiology, symptoms, and age. Management may be approached in the following manner:
- Diagnosis of atrial fibrillation
- Duration assessment
- Anticoagulation assessment
- Rate or rhythm control
- Treatment of underlying / associated diseases
This is part six of our series- Simplified in Practice where we break down ECG interpretation for various conditions. To read the earlier parts of the series, click here: Simplified in Practice: ECG basics & how to interpret, Simplified in Practice: How to detect myocardial ischaemia?, Simplified in Practice: Anterior Myocardial Infarction- Clinical nuggets on ECG characteristics, Simplified in Practice: What are the ECG changes when inferior STEMI starts?, Simplified in Practice: ECG features of posterior MI & Simplified in Practice: ECG nuggets in old STEMI (LV aneurysm)
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries