SCLC & NSCLC staging and treatment: What are the variables to be considered?- Dr. Ashok Komaranchath
M3 India Newsdesk Nov 25, 2020
This is the third article in the lung cancer awareness series where Dr. Ashok Komaranchath gives an overview of this challenging and critical topic and treatment of the disease, specifically staging and related treatment options.
Click to read other articles from Dr. Ashok Komaranchath.
We have discussed the basics of lung cancer, its types, clinical presentations and what sort of investigations are warranted. The treatment of lung cancer is complex and can involve medical oncologists, radiation oncologists, thoracic surgeons and surgical oncologists. There are many variables to be considered, especially in this era of personalised medicine. Since the topic is complex and extensive, I will try to be succinct and give an overview of the same.
By and large, the old sub-classification of lung cancer into small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC) is still a good starting point in deciding treatment.
Small cell lung cancer (SCLC)
This constitutes only 10 to 15% of all cases of lung cancer and is arguably the deadliest of the group. It is also a tumour with many peculiarities. One of its peculiarities is that it is so highly responsive to chemotherapy and radiotherapy that it has been described to ‘melt like ice in a hot sun’ when given treatment. The paradox is that, even in patients who achieve a complete response to treatment (no evidence of residual tumour on examinations or scans), the cancer recurs quickly and metastasises aggressively, killing the patient in a matter of months.
Another peculiarity is that this cancer is seen almost exclusively in smokers, with the dictum being, if SCLC is diagnosed in a non-smoker, it probably isn’t SCLC. Yet another quirk is that, even in the earliest stages of SCLC, there is no role for surgery. This is because it is considered such an aggressive disease that the cancer cells pass into the blood or lymph even at the earliest stage and any surgery done would ultimately be futile. Hence, the treatment is mostly by giving chemotherapy with or without radiotherapy.
The treatment depends on the stage, which is much simpler than most other cancers. It is divided into limited stage (all tumour within the range of a single radiation port) or extensive stage (extending beyond the field of possible radiation). I won’t be going into the specifics of the drugs used as it would be outside the scope of this article. Very recently, addition of a new modality called immunotherapy has been found to be beneficial in extensive stage SCLC.
Non-small cell lung cancer (NSCLC)
NSCLC is a much more heterogenous group of cancers where advances in pathology and molecular biology have paved the way for some impressive innovations in personalised cancer therapy. Arguably, the most important investigation in NSCLC is the biopsy. We need much more tissue than before to run the full gamut of histopathological and molecular tests than before. Hence, it is recommended that an FNA not be done for diagnosis of a suspected NSCLC. At least 2-3 cores of a tract biopsy would be adequate or a whole node excision biopsy would be even more ideal. Also, early stage (Stage I and II) NSCLC now have 5 year survival rates exceeding 60%. Before starting any treatment, it cannot be emphasised enough about the importance of a multi-disciplinary team approach to treatment and pre-treatment discussion with all team members as to the ideal steps of management of any stage of lung cancer.
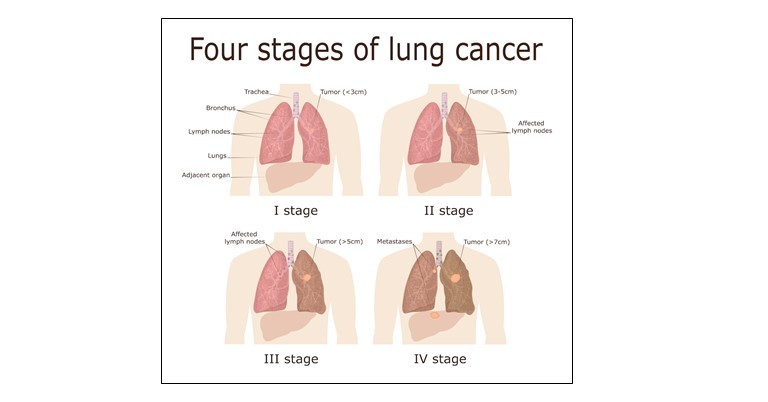
Stages of non-small cell lung cancer like most solid tumours are divided into four. A simplified version of the TNM staging system is given below:
- Stage 1: Cancer is found in the lung, but it has not spread outside the lung
- Stage 2: Cancer is found in the lung and nearby lymph nodes
- Stage 3: Cancer is in the lung and lymph nodes in the middle of the chest
- Stage 3A: Cancer is found in lymph nodes, but only on the same side of the chest where cancer first started growing
- Stage 3B: Cancer has spread to lymph nodes on the opposite side of the chest or to lymph nodes above the collarbone
- Stage 4: Cancer has spread to both lungs, into the area around the lungs, or to distant organs
Fig.1: Staging of non-small cell lung cancer [1]
STAGE I: In stage I NSCLC, standard of care is surgical resection. Surgical technique has also advanced greatly and concomitant morbidity and mortality have dropped significantly in the past few decades. However, a lobectomy is still preferred to a segmentectomy and in certain situations (e.g. a hilar mass) a pneumonectomy is also occasionally performed. If the patient is not a candidate for surgery, advanced radiation techniques like stereotactic ablative radiation (SABR) can be used with nearly equivalent efficacy to a thorough surgery. However, less than 10% of all cases are discovered in this stage.
STAGE II: Surgery remains the mainstay of therapy in stage II NSCLC also. However, as the likelihood of micro-metastases is higher, most patients are offered some form of adjuvant chemotherapy to prevent future recurrences. Post operative radiation is not offered routinely as trials have shown no added benefit and a possible inferiority to adjuvant chemotherapy.
STAGE III: This is the most controversial stage of NSCLC and the treatment options need to be carefully individualised to each patient after discussion with each member of the multi-disciplinary team as well as the patient and their relatives. If the lymph nodal spread of the tumour is low and the tumour is of a reasonably small size, surgery may still be an option, usually preceded by both chemotherapy and usually radiation as well.
But for most cases of stage III NSCLC, the treatment involves something called concurrent chemo-radiation. Here, the radiation oncologists mark out the areas to be irradiated using a pre-treatment CT scan, decide on the dose of radiation to be delivered and this information is fed to a planning computer. As the thorax is constantly moving with respiration, this movement is also taken into consideration and the radiation is delivered using a machine called the linear accelerator which accelerates subatomic particles which then strike the tumour releasing a certain measurable energy which causes damage to the cancer cells, both directly (DNA damage) and indirectly (free radical formation).
Chemotherapy is given at fixed intervals which potentiates the effect of this radiation, thereby leading to further damage and cell kill of the cancer cells. This form of treatment still provided only a 30% or less long term survival in stage III NSCLC patients. Recently, the advent of consolidation treatment with a new immunotherapy drug has seen the survival of these patients being improved spectacularly, with median progression-free survivals tripling and overall survival doubling. However, the exorbitant costs puts this new treatment out of the reach of many of our patients.
STAGE IV: Once the cancer has spread to the opposite lung, non-regional lymph nodes or other organs, it is called stage IV disease. There was a time not long ago, that a stage IV lung cancer patient was only sent home to die beside friends and family as he would probably live only for a few months after diagnosis.
In India, mainly due to the cost factor, it is common to see most of these patients started on chemotherapy alone. However, in an ideal situation, once stage IV is confirmed with a PETCT and an MRI of the brain, we assess the histology of the primary tumour. We also do multiple mutational analyses like EGFR, ALK, ROS1 and BRAF. Further treatment depends on these results. At the outset, if the MRI brain shows any metastases, it should be addressed first using either stereotactic RT or whole brain RT as decided by the radiation oncologist and the multi-disciplinary team.
- In case any of the above mutations are positive, we now have targeted therapy against each of these and in most cases are oral drugs which have been proven to be as or more effective than chemotherapy.
- In case they are negative, we do another immunohistochemistry test called PDL-1 which if positive (≥1%), paves the way for use of the newest and most effective weapon in our armamentarium; immunotherapy. Depending upon the level of positivity of PDL-1, we offer the patient either immunotherapeutics alone or a combination of immunotherapy and conventional chemotherapy.
The advent of immunotherapy has drastically improved survival in patients with Stage IV lung cancer by three to five fold as compared to conventional chemotherapy alone, and we now see patients routinely live past three years with a good quality of life. The side effect profile of immunotherapy is also vastly better than chemotherapy and is usually extremely well tolerated. The major drawback at this point of time is the exorbitant cost.
We will discuss more about some of the newer drugs available for advanced lung cancer and future prospects in the next and final article in this lung cancer awareness month series.
To read other articles in this series, click,
Lung cancer- Not a single disease: Dr. Ashok Komaranchath
Lung Cancer: The common clinical presentation and work-up for primary care: Dr. Ashok Komaranchath
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Ashok Komaranchath is a Medical Oncologist from Kerala.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries