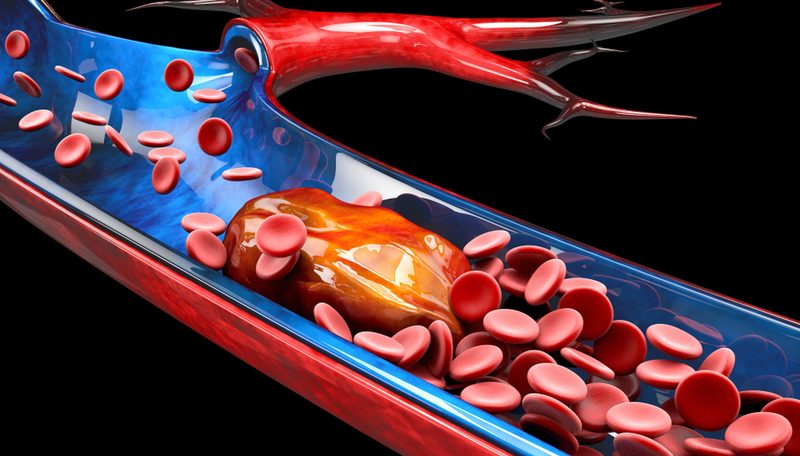
Artificial blood vessel gives glimpse into how blood clots form, resolve, and respond to blood thinners
American Society of Hematology Annual Meeting Press Release Dec 10, 2019
New technology is allowing researchers at the Emory University School of Medicine to grow blood clots in a controlled environment and examine the life-cycle of thrombosis that commonly leads to heart attack, stroke, pulmonary embolism, and other life-threatening events, to ultimately better target therapies. Researchers are using a novel assay, which they have dubbed a “vascular avatar” as a stand-in for an actual blood vessel to gather fundamental knowledge about how a thrombosis resolves and to test how different drugs or a cocktail of drugs might accelerate the process.
 “The way we typically treat blood clots is to give medicines that cause someone to bleed to restore blood flow and avoid ischemic injury, but we don’t want to cause excess bleeding, so it’s always this delicate balance,” said lead study author Yongzhi Qiu, PhD. “This is the first assay to allow us to really understand what happens during the lifetime of a clot – looking at it from the time it forms, to see how clots get better, either on their own or when adding different clot-busting drugs.”
“The way we typically treat blood clots is to give medicines that cause someone to bleed to restore blood flow and avoid ischemic injury, but we don’t want to cause excess bleeding, so it’s always this delicate balance,” said lead study author Yongzhi Qiu, PhD. “This is the first assay to allow us to really understand what happens during the lifetime of a clot – looking at it from the time it forms, to see how clots get better, either on their own or when adding different clot-busting drugs.”
With this technology, the team engineered microvasculature on a chip. It is similar to when skin cells are cultured on a two-dimensional slide, but here researchers grow endothelial or blood vessel cells in a tissue-like material to form a three-dimensional micro-vessel with branches in a petri dish. The technology models the biophysical microenvironment, such as vessel size, geometry, wall stress, and the tissue stiffness surrounding the blood vessels. The artificial blood vessels are grown over several weeks and the clots are then studied over days to weeks, which mirrors the typical duration seen in patients. The researchers are able to examine how the cellular and biochemical composition of the clot changes and how hemodynamics (blood flow) affect the process.
Dr. Qiu said they have already made some interesting discoveries. For example, inflammation seems to induce protein deposits that initiate clot formation. As clots start to resolve, platelets are mostly undetectable after one day. In addition, if blood vessels are less inflamed, endothelial barrier function restores in one day after the inflammatory insults are removed, and the clots resolve in about 10-14 days. However, if blood vessels are severely inflamed, neutrophils and fibrin persist and may continue to block blood flow and prevent blood vessel cells from recovering. Researchers explained that this may suggest that clinicians do not need to be as hesitant to give anti-platelet therapy before clots form and that not all blood clots are the same.
They said that this assay may warrant broad application in studying thrombosis associated with inflammation that occurs in many conditions such as lupus, rheumatoid arthritis, inflammatory bowel disease, or other autoimmune diseases, as well as many cancers.
“This is the first time we’ve been able to look at the clot for this long of a duration and under these controlled circumstances to model different disease states. What we are learning is that not all clots are created equal, and not all clots should receive the same type of therapy – some therapies are going to be better for certain clots than others,” Dr. Qiu said. “We’re also seeing that certain antithrombotic medications seem to improve the leakiness of the blood vessel cells so not only is it busting the clot, it’s also helping the blood vessel get better.”
He said the implications of this finding are fairly broad because it could mean that even if a person does not have a clot yet, but they have evidence of inflammation, anticlotting medication may play a role in preventing blood clotting and may keep the blood vessel healthier. Clot resolution also appears to be dependent on the extent of inflammation, suggesting that the application of anti-inflammatory medicine might facilitate the clot resolution. Of course, more study is needed.
The researchers say they are hopeful that this assay may help clinicians better target anti-thrombotic and anticoagulant therapies and open new opportunities for therapeutic interventions. They are looking into how to scale the technology for broader use.
This study was funded by grants from the National Institutes of Health.
This article is a news release from American Society of Hematology Annual Press Meeting. Read the original here.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries