Urogenital Anomalies of Newborns: Assessment and Management Approach
M3 India Newsdesk Mar 10, 2023
Congenital urogenital anomalies are birth defects and inherited conditions that affect the urinary tract or the genital tract. Here the author has penned down the common anomalies in newborns that could be diagnosed in the neonatal period.
ATTENTION: Images in this article contain pictures of newborn presentation which some people may find offensive or disturbing. Viewer discretion is advised.
The genitourinary problem is quite common. Development of the urinary tract and genital tract are closely linked. Some of these undiagnosed cases have huge repercussions in the form of significant morbidity and mortality. Antenatal sonography is of great significance to diagnose congenital abnormalities of the kidney and urinary tract (CAKUT). Most of these defects are structural and need corrective surgery, necessitating the need for early identification and timely referral by general paediatricians.
We would be discussing common anomalies under the following headings:
- Penile and urethral anomalies
- Testicular and scrotal anomalies
- Vaginal anomalies
- Disorders of sex development
1. Penile and urethral anomalies
- Foreskin variant: Normal baby has preputial adhesions which are physiological till 6 years, limiting the view of the urethral. No intervention is needed.
- Buried penis: Normally developed penis camouflaged by suprapubic fat. Surgical repair is indicated in case of a splayed urinary stream or for cosmetic concerns.
- Hypospadias with/without chordee: Urethral meatus placed ventral aspect, more proximal anywhere between glans to the perineum. Classified according to the position of the meatal opening as glandular (on the glans penis), coronal, sub-coronal, mid-penile, penoscrotal, scrotal and perineal (Fig. 1). Depending on the severity as suggested by the proximalisation and association of hypospadias with chordee (ventral penile curvature), surgical correction is warranted. The ideal age of repair is 6 to 12 months. Circumcision is contraindicated as the foreskin is required for most of the repair. DSD should be suspected in newborns with proximal hypospadias along with cryptorchidism.
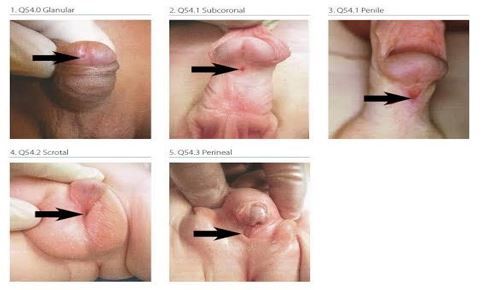
Fig. 1: Types of hypospadias (click on the image to view)
- Epispadias: Rare urogenital anomaly characterised by failure of the urethral tube to tabulation on the dorsal aspect leading to the ventral placement of the urethral opening. Commonly associated with severe exstrophy-epispadias complex, affecting 1 in 117,000 males and 1 in 480,000 females.
Apart from the obvious anomaly of the meatal anomaly, males have short and upward pointing phallus and ventral hooding of the prepuce. Alike males, females also have certain anatomic abnormalities in the form of a bifid clitoris, patulous urethral opening, anteriorly placed vaginal opening and ill-formed or absent mons (Fig. 2). Total urinary incontinence is present in proximal epispadias (in males) and in all females with epispadias due to a wide urethral plate and underdeveloped sphincter. Surgical management is quite challenging. Corrective surgery warranted by the age of 6-12 months, done in a staged approach. It aims at restoring the normal anatomy of genitalia and urethral with bladder neck reconstruction to attain continence.

Fig. 2: Epispadias- Exstrophy complex (click on the image to view)
2. Testicular and scrotal anomalies
A. Inguinal hernia: Congenital inguinal hernia is quite common, with an incidence of 1 to 4 % in term and 30% in preterms, with a male-to-female ratio of 6:1. Visible as a swelling in the inguinoscrotal region because of the protrusion of intraabdominal content through patent processes vaginalis. Presents as a bulge in the groin on crying and straining.
On examination: Cough/ strain impulse could be elicited, can’t get above the swelling, testis felt separate from the swelling. Should be differentiated from the undescended testis and retractile testis. Requires elective surgical repair (herniotomy) once a definitive diagnosis is made. Day care procedure where hernia sac is ligated at the deep inguinal ring. Timely repair prevents the future risk of incarceration.
B. Hydrocele: Accumulation of fluid in between the layers of tunica vaginalis. Scrotum appears enlarged, and non-tender. On examination: Transillumination test positive (Fig. 3), one can get above the swelling. Watchful waiting is advised as most would resolve spontaneously by 12 months. Those which fail to resolve or are very tense require elective surgical repair. Hydrocele fluid is drained and high ligation of processes vaginalis done similar to the repair of indirect inguinal hernia.

Fig. 3: Positive transillumination test (click on the image to view)
C. Cryptorchidism: By definition, this means the absence of a palpable testis in the scrotum. It comprises UDT (undescended testis), ectopic testis, atrophic testis and retractile testis.
i. UDT: Failure of descent of the testis along its normal pathway from the retroperitoneum to the scrotum. At birth, UDT has an incidence of 4.5% in term males and 30% in preterm males, usually unilateral (bilateral in 10% of cases). Testis which failed to descend along its normal pathway from the retroperitoneal to the scrotum. Classified as abdominal, peeping, inguinal, gliding and ectopic. Testis that fails to resolve by 3 months requires bilateral orchiopexy to prevent potential consequences (poor testicular growth, infertility, testicular malignancy, associated hernia, torsion of the cryptorchid testis, and the possible psychological effects of an empty scrotum).
ii. Retractile testis: May be diagnosed as undescended testis. Due to the brisk cremasteric reflex in young children, the testis could be positioned in the supra-scrotal region. The examination was done in a relaxed frog-leg position. The retractile testis can be manipulated into the scrotum comfortably. Follow-up should be done every 6-12 months as there is a future risk of becoming acquired undescended testis.
3. Vaginal anomalies
Para urethral cyst: In newborn girls, it results from retained secretions in the skene glands secondary to ductal obstruction. Mostly resolve spontaneously during first 4-8 weeks (rarely requires incision & drainage).
4. Disorders of sex development
A condition that comprises a heterogeneous group of disorders caused by the atypical development of chromosomal, gonadal or anatomical sex. Considering the demography of society, it is more of a social emergency than medical urgency.
Newborns with the following findings require a thorough evaluation to diagnose life-threatening conditions such as CAH and for assigning the sex.
- Ambiguous genitalia
- A penis and bilateral cryptorchidism
- Unilateral cryptorchidism with hypospadias
- Severe proximal hypospadias (penoscrotal, scrotal or perineal) with or without microphallus with normally descended testis
- Apparently female genitalia with clitoromegaly and / inguinal hernia or palpable gonadal
- Asymmetry of size, pigmentation or rigatoni of labioscrotal folds
- Discordant of external genitalia with prenatal karyotype
The detailed evaluation and management have not been discussed in the current article. As general paediatricians, we must be aware of the possible clinical clues that could ignite and expedite the need for further workup. So that neither the underlying medical illness nor the parental dilemma could be addressed suitably.
To summarise, ultrasonography of the KUB region should be done to diagnose any other associated abnormality in newborns with the significant genitourinary problems discussed above. Although the management of genitourinary problems requires surgical proficiency by exemplary pediatric surgeons and urologists. Still, general paediatricians are the one that bears the sole responsibility to initiate the journey for corrective intervention.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Sakshi Bhuddi is a community health paediatrician from Nainital.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries