Understanding Deep Brain Stimulation (DBS) Therapy for Parkinson's: Patient Selection and Outcomes
M3 India Newsdesk Apr 11, 2024
This article outlines the use of Deep Brain Stimulation (DBS) as a treatment option for medication-refractory Parkinson's Disease. It also emphasises patient selection criteria, surgical procedures, potential outcomes, and future developments.
Case study
A 55-year-old lady was suffering from progressively worsening symptoms of Parkinson’s Disease. Initially, she had symptoms of stiffness, rigidity, bilateral asymmetric rest tremors and reduced arm swing. Anti-parkinsonian medications did significantly improve her rigidity and bradykinesia; however, her tremors seemed to be refractory as she continued to have tremors despite adequate medical therapy.
Deep Brain Stimulation(DBS) refers to an implantable system which delivers electrical impulses to specific parts of the brain to modulate neurological symptoms not amenable to medical therapy. DBS is both adjustable and reversible in nature1.
Indications for DBS in Parkinson’s Disease (PD)
Briefly, DBS is indicated for the following three major disabilities in patients with PD:
- Disabling and prolonged off state.
- Persistent dyskinesias despite optimal therapy.
- Tremor not responsive to medical therapy.
The following are the symptoms of PD which are responsive to DBS:
Responsive Parkinson's Disease Symptoms
Motor symptoms that respond to the best state:
- Rigidity
- Tremor
- Bradykinesia
- Dyskinesias
- Dystonia(If not fixed)
- Motor fluctuations, including dose wearing off, on-off, and dose failures
- Sleep, including architecture and efficiency
Symptoms of PD unresponsive to DBS include:
- Unresponsive Parkinson's Disease Symptoms
- Sleed (may worsen)
- Cognition
- Gait and postural instability (if not levodopa responsive)
- Autonomic symptoms
- Mood and behaviour: Can improve or worsen
Patient selection for DBS in PD
The Core Assessment Program for Surgical Interventional Therapies in Parkinson’s Disease (CAPSIT-PD)2 was designed to guide while selecting PD patients for DBS. It included the following recommendations:
- The patient should have a diagnosis of Idiopathic PD and a minimum duration of illness of 5 years (to exclude the possibility of evolution into Atypical PD variants).
- Dopamine responsiveness should be confirmed by a dopamine or apomorphine test, demonstrating a 33% increase in the Unified Parkinson Disease Rating Scale (UPDRS) part III score.
- Patients having a major cognitive impairment and/or severe depression must be screened as they are not suitable candidates for DBS.
Hence the ideal PD patients suitable for DBS are younger, have little or no cognitive impairment, have fluctuating motor symptoms and are at high functioning when their medications are optimised.
Mechanism of DBS
The exact mechanism of action of DBS is yet unknown. Some of the postulated mechanisms are as follows:
- Microlesion
- “Jamming” or disrupting networks
- Depolarisation Blocks
- Preferential large axon activation
- Stimulation-induced release of GABA, Adenosine
- Stimulation-induced modulation of pathological network activity
- Activation and excitation of the target nucleus
- Increased ATP release followed by accumulation of its catabolic product, Adenosine
Targets for DBS in PD
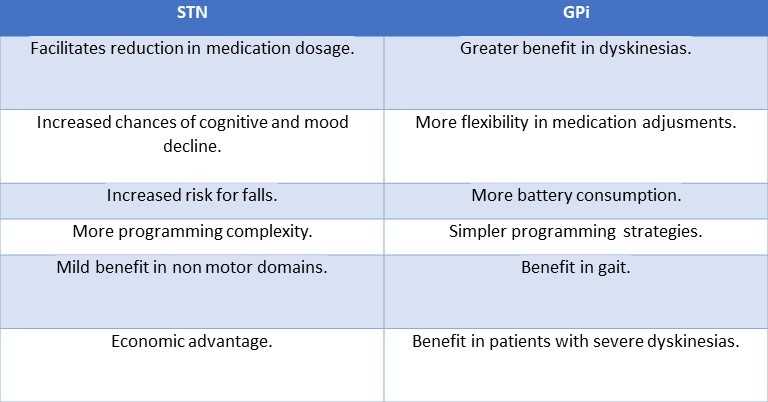
The STN (Subthalamic Nucleus) and GPi (Globus Pallidus interna) are the currently preferred targets for DBS in medication-refractory PD. The advantages and disadvantages of stimulating both these areas are summarised in the table below:
DBS procedure (in brief)
The selected patient undergoes a baseline high-resolution MRI of the brain to identify the stereotactic target. Dopaminergic medications are stopped 12 hours before the procedure.
A stereotactic head frame is placed on the patient’s head under local anaesthesia. Using reference points from brain imaging, this frame is used to create a virtual three-dimensional space which is used to identify the desired target.
Various neurophysiological techniques (e.g. microelectrode recording (MER), microelectrode stimulation and macro electrode stimulation) are used by various centres to ensure correct mapping of the target region.
The nuclei of the basal ganglia region (STN, thalamus, GPi) have a sensorimotor region which needs to be accurately stimulated by the electrode to avoid untoward neuropsychiatric side effects. Also, stimulation of surrounding tracts and white matter should be avoided.
The DBS lead is placed in the target location and subsequently macro stimulation is performed to check for effects and side effects.
Commonly observed side effects due to stimulation of adjacent structures include:
- Twitching or tonic contractions of the face or limbs (internal capsule)
- Dysarthria (corticobulbar fibres)
- Paresthesias (medial lemniscus or sensory areas)
- Unilateral pupillary changes or eye deviation (tracts involving ocular function)
- Phosphenes/flashes of light (optic tract region)
The presence/absence of these side effects may lead the surgeon to adjust the lead position.
Post-operatively patients are discharged on their previous medications and are summoned later for implanted pulse generator (IPG) implantation and programming.
The IPG is implanted in the anterior chest wall and stimulation parameters can be subsequently adjusted. Programming is done to identify optimum programming parameters (polarity, frequency, pulse width, and voltage), monitor for side effects and optimise medications.
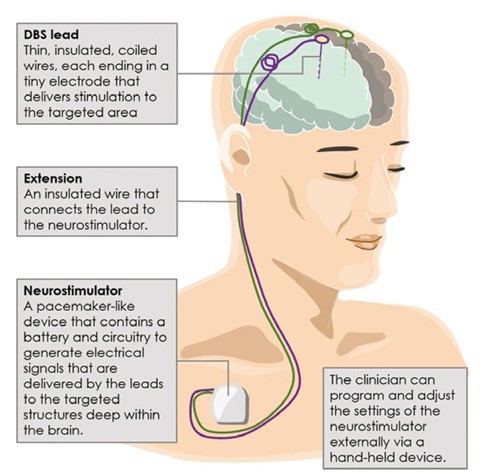
At present, only “open-loop” neurostimulation is performed using DBS, meaning the stimulation continues using the previously set parameters without sensing brain signals5. In future, “closed-loop” stimulation may be developed in which local field potentials of the target are recorded by the implanted electrode which will modulate the stimulation accordingly.
Outcomes of DBS surgery
- Most multicentre trials have reported that daily off time and dyskinesias are improved by subthalamic nucleus (STN) stimulation6.
- The STN target is associated with greater medication reduction, while the GPi target is better at addressing dyskinesias.
- Psychiatric adverse effects related to STN include worsening of depression, anxiety, and impulse control disorders.
- Some patients can have worsening gait, speech disturbances and persistent freezing of gait not responsive to levodopa.
Conclusion
DBS is being increasingly used nowadays for the treatment of medication-refractory PD. As more centres are beginning to provide DBS, quality control and the development of a standard of care increase.
Patient education before DBS is of utmost importance to make them aware of possible outcomes and complications and avoid unrealistic expectations from patients and their caregivers.
The patient who desired to have better control over her tremors was offered the option of DBS. The patient was relatively young, without major medical comorbidities with intact cognition. Post DBS she attained significant improvement in her tremors and could even reduce her antiparkinsonian medication dosage while she maintained her normal daily activities.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Annesh Bhattacharjee is a Consultant Neurologist, at Dept. of Neurology GNRC Hospital, Guwahati.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries