Type 1 Diabetes: ISPAD Guideline Updates- Part 2
M3 India Newsdesk Dec 20, 2023
The article offers comprehensive guidelines for managing diabetes in children & adolescents, focusing on the use of technology to reduce complications. It covers screening recommendations, exercise guidelines, diabetes technologies, sick day management & considerations for limited resource settings.
The new guidelines focus on a holistic approach to managing diabetes in children and adolescents. They emphasise the use of technology to reduce the complications associated with long-term glycemic variability in patients with type 1 diabetes.
Microvascular and macrovascular complications in children and adolescents with diabetes
Screening for diabetic complications in T1D as a rule should start at puberty or from age 11 years, whichever is earlier or with 2-5 years of diabetes duration, and repeated annually thereafter. Screening for T2D should start at diabetes diagnosis and then be repeated annually. Prevention or cessation of smoking will reduce the progression of albuminuria and CVD.
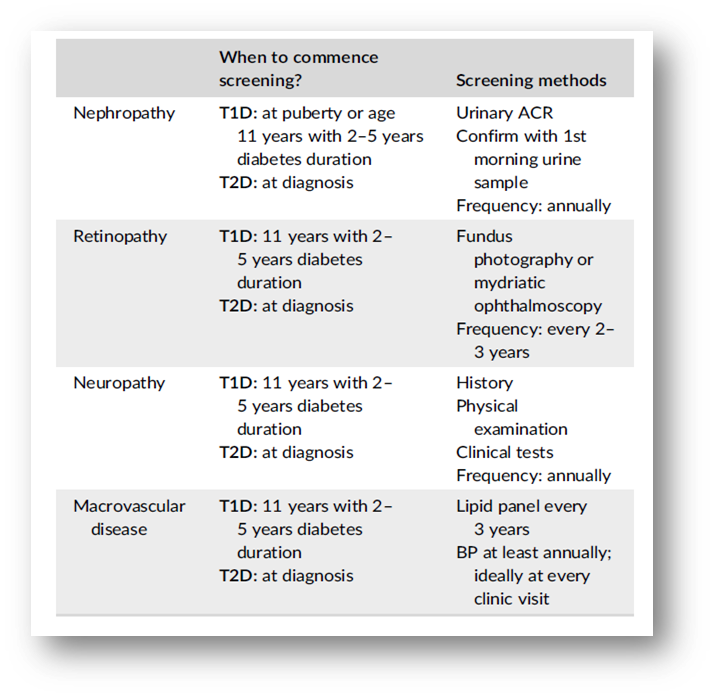
Screening recommendations for vascular complications
Albuminuria
Consider confirming persistently increased albuminuria by the first-morning urine sample for urinary albumin/creatinine ratio (ACR) to rule out orthostatic proteinuria. It is recommended to use 2 of 3 urine samples over a 3–6-month period as evidence of increased albuminuria.
Optimise blood pressure (BP) to prevent the onset and progression of albuminuria. Consider ACE inhibitors or ARB in adolescents with persistently elevated albuminuria to prevent progression to proteinuria.
Monitoring for changes in BP, serum creatinine and potassium within 2 weeks of initiation of an ACE inhibitor or ARB, and annually thereafter.
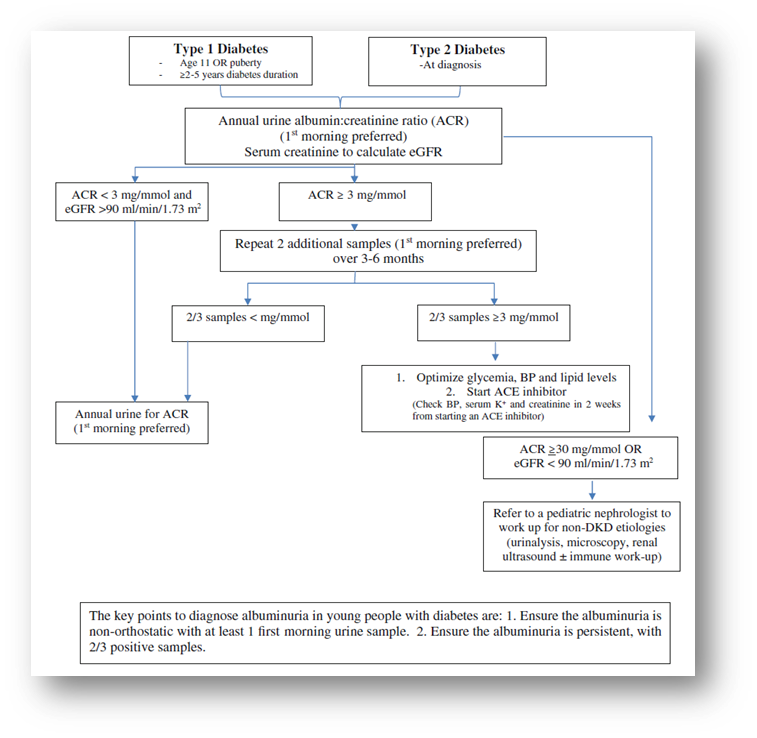
Diabetic kidney screening algorithm for a young person with T1D and T2D
Retinopathy
For those with diabetes <10 years, mild non-proliferative DR (NPDR, i.e., microaneurysms only) and optimal glycemic targets, a biennial screening assessment is recommended. The frequency of retinopathy screening can be reduced to 3 years if there is no retinopathy at first assessment but needs to be more frequent if there are high-risk features for visual loss.
Laser treatment and intravitreal injections of anti-VEGF agents reduce the rate of visual loss for individuals with vision-threatening stages of retinopathy (severe NPDR or worse and/or DME).
Neuropathy
Screening for peripheral neuropathy includes assessment of temperature or pinprick sensation, vibration and ankle reflexes. Screening for cardiac autonomic neuropathy includes assessment of orthostasis and heart rate variability (HRV).
Blood pressure
For people with diabetes <13 years of age hypertension is defined as average systolic (SBP) and/or diastolic BP (DBP) ≥ 95th percentile for sex, age, and height on three or more occasions. For people with diabetes ≥13 years of age, hypertension is defined as average SBP and/or DBP ≥130/80 mm Hg.
Initial treatment of hypertension consists of weight loss, limitation of dietary salt, and increased physical activity. If unable to achieve normal BP after 6 months of lifestyle interventions start with ACE inhibitors or ARB.
Lipids
Screening with a fasting lipid profile is ideal but often not practical in youth with diabetes. Non-fasting lipids screening may be obtained and if triglycerides or LDL levels are elevated, a fasting lipid profile would then be indicated.
Lifestyle modification remains the first choice for treating dyslipidemia until the patient has a history of familial hypercholesterolemia. If the above interventions do not lower LDL cholesterol <3.4 mmol/L (130 mg/dL), statins may be considered in children from age 10 years.
Other complications and associated conditions in children and adolescents with type 1 diabetes
- Screening for thyroid disease by measurement of TSH, anti-thyroid peroxidase antibodies and anti-thyroglobulin antibodies is recommended soon after diagnosis of diabetes once the individual is clinically stable. Thereafter, TSH should be measured every second year in asymptomatic individuals and every year in individuals with positive antibodies at diagnosis or a family h/o autoimmune thyroid disease.
- Screening for Coeliac disease (CD) is recommended during the initial year of diabetes diagnosis and at 2–5 years intervals. Children with CD should have annual screening for thyroid function and monitoring of vitamin D to optimise bone health.
- Education regarding proper injection technique, rotation of injection sites with each injection and non-reuse of needles remain the best strategies to prevent lipo hypertrophy (LH) and lipoatrophy (LA). Injection sites should be regularly assessed at each clinic visit for LH and LA as they are potential causes of glucose variability.
Exercise in children and adolescents with diabetes
- As per recommendation, 60 minutes of moderate and vigorous physical activity is advised, and exercise is a cornerstone in the management and mitigation of cardio-metabolic risk factors for children and adolescents with T1D and type 2 diabetes (T2D). High-intensity exercise is generally contraindicated in those with more advanced or proliferative retinopathy.
- During all forms of physical exercise high glycemic index carbohydrates should be available to prevent and treat hypoglycemia. Regular monitoring with SMBG and CGM should be encouraged.
- A wide range of insulin adjustment and nutrition strategies can be combined to keep the glucose level in the exercise range of 5.0–15.0 mmol/L or 90–270 mg/dl and prevent exercise-induced hypoglycemia.
- Exercise in children and adolescents with T1D and T2D is contraindicated in the presence of blood ketones ≥1.5 mmol/L or urine ketones: 2+ or 4.0 mmol/L. If blood ketone levels are between 0.6 and 1.4 mmol/L, exercise should be postponed until the cause of elevated ketone levels has been evaluated and an insulin bolus dose is given equally to half the usual individual correction dose (or 0.05 U/kg).
- Insulin dose adjustments are mostly required for aerobic exercise, and less likely required for very high-intensity or anaerobic exercise which is more commonly associated with elevated glucose levels.
Diabetes technologies: Glucose monitoring
- Regular self-monitoring of glucose is essential for diabetes management for all children and adolescents with diabetes.
- The use of CGM or SMBG (for low-resource settings) is strongly recommended in all children, adolescents, and young adults with T1D.
Diabetes technologies: Insulin delivery
- Connected insulin pens have the potential to improve diabetes management through intensive insulin therapy with multiple daily injections (MDI). Connected pens if available may be offered to interested youth who prefer not to have an on‐body device.
- Continuous subcutaneous insulin infusion (CSII) (pump) therapy is recommended and appropriate for youth with diabetes, regardless of age.
- Not‐integrated insulin pump therapy is safe and effective in youth with type 1 diabetes (T1D) to assist with achieving glycemic targets.
- Sensor-augmented pump (SAP) therapy is superior to MDI with Self-monitoring of blood glucose (SMBG) in reducing HbA1c without an increase in hypoglycemia or severe hypoglycemia.
- Closed-loop systems are strongly recommended for youth with diabetes. It improves time in range (TIR) by minimising hypoglycaemia and hyperglycemia.
Sick day management in children and adolescents with diabetes
Children should be taught to proactively adjust diabetes therapy to prevent uncontrolled or symptomatic hyperglycemia, dehydration, hyperglycemic ketosis, ketoacidosis, hypo-normoglycemic ketosis, and/or severe hypoglycaemia. Never completely stop insulin! The aim of management should be to avoid the development of ketosis.
- Always monitor glucose, defined as either blood or interstitial glucose, and ketone levels at least every 1–2 h.
- Monitoring blood ketones is preferred over urine ketones. Blood ketone monitoring during illness can reduce emergency room visits and hospitalisations.
- Aim for glucose levels between 3.9 and 10 mmol/L (70–180 mg/ dl) and blood ketones below 0.6 mmol/L.
- If available, continuous glucose monitoring (CGM) devices or intermittently scanned glucose monitoring (isCGM) devices can preferably be used to supplement blood glucose monitoring.
Ramadan and other religious fasting by young people with diabetes
Pre-fasting counselling is a must for young people wishing to fast and the necessity of SMBG and insulin injection during fasting to prevent acute complications is important. Frequent SMBG or CGM is recommended during fasting to minimise the risk of hypoglycemia and detect periods of hyperglycemia.
Consider meals based on low GI carbohydrates and include fruit, vegetables, and lean proteins. MUFA and PUFA should be used instead of saturated fats. Sweets and fried foods should be limited, and sweetened drinks avoided. For Ramadan fasting, consider consuming the pre-dawn meal (Suhor) as late as possible. Hydration should be maintained.
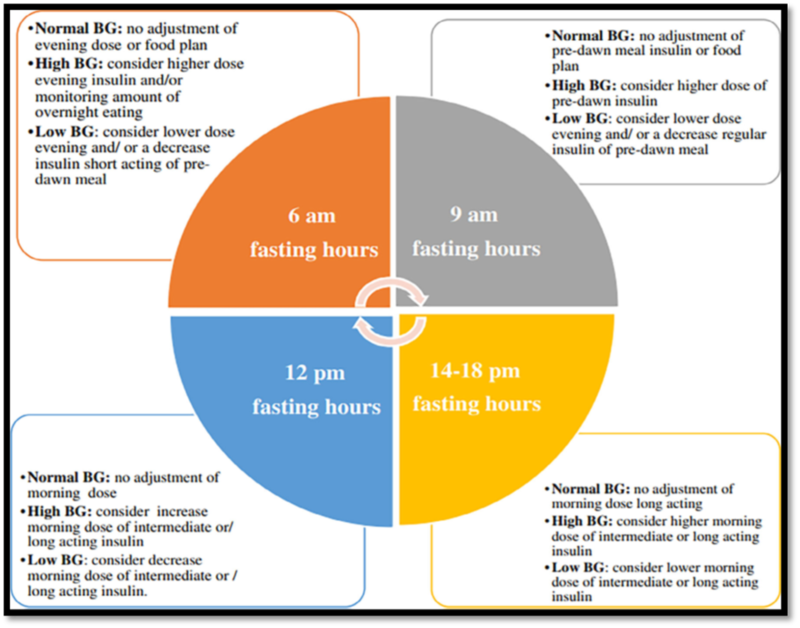
Schematic adjustments of insulin dose and/or food considerations during fasting hours
Management of the child, adolescent, and young adult with diabetes in limited resource settings (LRS)
- Diabetes management in LRS should be as physiological as possible, maximising quality of life (QoL), preventing acute and chronic complications, and allowing adequate growth and development.
- The diagnostic criteria for all types of diabetes are based on symptoms and laboratory measurements of BGL. If BGL testing is unavailable, diabetes can be provisionally diagnosed if classical symptoms are present and urine glucose is elevated (and urine ketones are present, if testing is available).
- Measurement of islet autoantibodies, C-peptide or genetic tests is not routinely recommended for the diagnosis of T1D. They may be selectively done if the diabetes type is unclear.
- Optimal glycemic targets and QoL can be achieved using low-cost conventional insulin (Regular and NPH) and SMBG, though analogue insulin offers some advantages.
- Pre-mixed insulin and two-dose regimens are not physiological. They are associated with increased acute and chronic complications, offsetting financial benefits, if any. Hence, these are not desirable for the management of T1D and should only be used until other alternatives can be obtained.
- Though glucose monitoring is expensive, the achievement of glycemic targets is not possible without regular SMBG. If the idea of 6–10 SMBG tests per day is not possible, at least pre-meals and bedtime BGL testing are suggested for determining appropriate insulin dosing and reducing nocturnal hypoglycemia.
- Target HbA1c for young PwD should be <7.0% (<53 mmol/mol) without frequent hypoglycemia and/or severe hypoglycemia (SH), although targets may need to be individualised based on circumstances.
- DKA may be more common in LRS, due to inadequate awareness, misinformation, and barriers to accessing care. Mild and moderate uncomplicated DKA can be treated with subcutaneous (SC) Regular insulin (or rapid-acting insulin analogues, if available and affordable). Severe DKA should be managed at the tertiary centre.
- In youth with type 2 diabetes metformin is the initial therapy of choice. If HbA1c is >8.5% and ketones are present, long- or intermediate-acting insulin should be prescribed initially.
- If islet autoantibody testing is not available, then family history, evidence of insulin resistance (acanthosis, skin tags) and the course of diabetes may provide clues to the diagnosis and whether long-term insulin is needed.
Click here to read: Type 1 Diabetes: ISPAD Guideline Updates- Part 1
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries