Transvaginal Sonography During Pregnancy
M3 India Newsdesk Jul 03, 2023
Ultrasound is an invaluable imaging tool and practically all obstetric imaging is done using ultrasound with MRI used in limited cases as a problem-solving tool. This article explains the technique of Transvaginal ultrasound (TVS) along with its clinical scenarios in the 1st trimester.
Transabdominal ultrasound (TAS)
In our country, pelvic ultrasound is routinely performed by the transabdominal (TAS) route. However, TAS has a few disadvantages which include:
- TAS is done using a low-frequency convex probe which offers a limited resolution.
- Thick maternal anterior abdominal wall degrades the image resolution further in obese patients.
- Distended urinary bladder, which is required as an acoustic window to displace the gut loops which come in between the ultrasound probe and the uterus also degrades the resolution. A distended urinary bladder is also not comfortable and leads to increased wait time for the patient.
Transvaginal ultrasound (TVS)
Transvaginal ultrasound (TVS) overcomes these disadvantages. A higher frequency can lead to much better resolution since the probe is closer to the imaged organs. Also, no other intervening tissues, like the abdominal wall, degrade the image resolution. TVS requires a contracted urinary bladder which is comfortable for the patient.
The technique of TVS
After emptying her bladder, the patient is put in a dorsal lithotomy position. The endocavitary transducer is covered with a clean probe cover or a condom. Water-soluble lubricant or sterile water should be used on the exterior of the transducer cover. The transducer is gently introduced into the vagina to reveal the relevant structures. Post imaging, the transducer should be disinfected per local disinfection standards.
Ideally, the first-trimester ultrasound should be done in the late first trimester, between 11 and 14 weeks, as risk assessment for trisomies and preeclampsia can also be performed during this period.
Typical clinical scenarios for TVS in the first trimester
1. Pregnancy with bleeding p/v or spotting
The possible scenarios are:
- Normal intrauterine pregnancy- Early intrauterine pregnancy will show a small cystic structure showing a double decidual sac sign in the uterine cavity. The presence of a yolk sac and fetal node within the cystic structure is confirmatory of intrauterine pregnancy. Cardiac activity is often seen when the embryo is greater than 2 mm in size and indicates viability.
- Early pregnancy failure- Gestational sac > 16mm in size showing no fetal node on TVS suggests early pregnancy failure, whereas on TAS, the gestational sac size should be >25mm to diagnose early pregnancy failure. With TVS, it is possible to diagnose pregnancy failure early
A gestational sac with an embryo > 7mm and showing no cardiac activity is confirmatory of early pregnancy failure. - Ectopic gestation- Most ectopic gestations occur in the fallopian tube. TVS is much superior to TAS in identifying ectopic pregnancy at the earliest, which makes a significant difference in the management of the patient. Typical findings in ectopic gestation are heterogeneous lesions in the adnexa consisting of blood clots and the gestational sac with free fluid in the pelvis and the abdomen. Less commonly, the gestational sac with a live embryo may be identified. Nontubal ectopic pregnancy may occur in the ovary, cervix, cesarean section scar, or rarely intra-abdominal. TVS plays an important role in determining these conditions.
- Rarely molar pregnancy / Hydropic degeneration of villi- It will show an echogenic mass with numerous internal cysts in the uterine cavity.
2. Dating of pregnancy in a lady with irregular periods / unknown LMP
Crown-rump length is the most accurate biometry measurement to date in pregnancy and it is better done with TVS than TAS. The accuracy is more in early pregnancy. The initial age assignment should not be revised on subsequent scans. Overall, the accuracy of sonographic dating in the first trimester is ~5 days (95% confidence range)
3. Confirming the number of pregnancies
First-trimester ultrasound is very accurate in identifying multiple pregnancies and determining the chorionicity and amnionicity which is of utmost importance in managing the pregnancy.
4. Antenatal screening for aneuploidy
Nuchal transluceny (NT), Nasal bone ossification, foetal heart rate and maternal age is used for risk estimation for trisomies between 11 - 14 weeks. This can be done transabdominally or transvaginally.
5. Early detection of anomalies
Few anomalies like acrania, alobar holoprosencephaly, open spinal bifida etc can be diagnosed in the first trimester using high-end imaging equipment.
Indications for TVS in 2nd and 3rd trimester
- Access the cervical length and incompetence
- Accurately identify the lower margin of the placenta and placenta praevia
- Access the lower uterine segment and LSCS scar thickness
- Better access to the structures/anomalies in a few circumstances
Case Studies
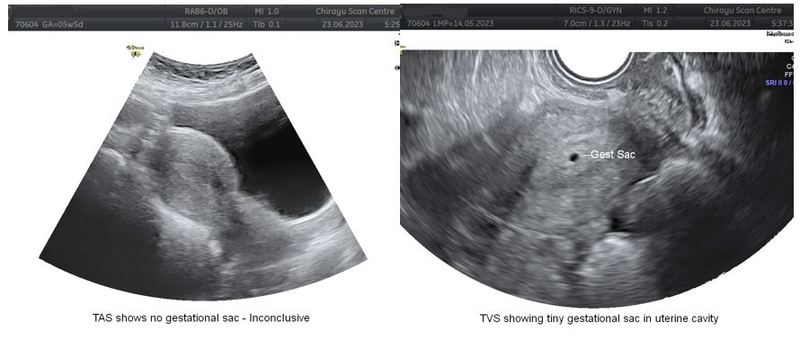
Case 1Mrs. X, 28Y/F G2, P1, L1 with amenorrhea of 40 days and +ve UPT, presented with bleeding p/v and mild cramping for one day. TAS showed an empty uterine cavity, normal adnexa, and no free fluid in POD. Here TAS is inconclusive with three possibilities – Early intra-uterine pregnancy, Complete abortion, or Ectopic gestation. Without TVS, the recommendation is to repeat the ultrasound in 1 week / SOS. TVS showed a tiny gestational sac measuring about 3mm in the uterine cavity, giving a definite diagnosis of early intra-uterine gestation.
Case 2
Mrs Y, 30/F, G2, P1, L1 was referred for an anomaly scan. TAS was suspicious for funnelling at internal os. TVS clearly showed the funnelling and shortened cervix.

In conclusion, TVS is superior to TAS in early pregnancy and essentially all first trimester (<13 weeks) ultrasound can be and ideally should be done transvaginally.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ashoka GK is a practising Radiologist at Chirayu Scan Centre, Puttur, Karnataka.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries