Subacute and Chronic Cough in Adults
M3 India Newsdesk Dec 03, 2023
This article emphasises the significance of obtaining medical evaluation for proper diagnosis and management and provides a thorough overview of acute, subacute, and chronic coughs.
Coughing, a reflex action aiding in clearing the airways, it performs an essential protective function for human airways and lungs, it is a common respiratory symptom. It can be brief or persist for extended periods, leading to discomfort and concern. Categorising coughs based on their duration acute, subacute, and chronic helps in understanding their underlying causes and appropriate management.
Definition of acute, subacute, and chronic cough
1. Acute cough: Typically lasts for less than three weeks(< 3 weeks), often a response to a viral upper respiratory tract infection. It can also result from exposure to irritants or allergens, aspiration, inhalation of noxious chemicals or smoke
2. Subacute cough: Extends beyond three weeks but lasts less than eight weeks (3-8 weeks). It might stem from a lingering respiratory infection or initial phases of a chronic condition it is a common residuum of tracheobronchitis, as in pertussis or “postviral tussive syndrome”
3. Chronic cough: Persists for more than eight weeks(>8 weeks) and demands thorough investigation. A wide variety of cardiopulmonary diseases, including those of inflammatory, infectious, neoplastic and cardiovascular etiologies. It could signify various underlying issues, ranging from respiratory diseases to gastrointestinal reflux or medication side effects (ACE inhibitors).
Causes of subacute and chronic cough
- Respiratory infections: Prolonged coughing after an initial illness can be a sign of a lingering infection, such as bronchitis or pneumonia. And in India, we should not forget about tuberculosis
- Asthma: Both subacute and chronic cough might be an indication of asthma, especially when accompanied by other symptoms like wheezing or shortness of breath.
- Gastroesophageal Reflux Disease (GERD): Stomach acid backing up into the oesophagus can trigger coughing, particularly when lying down or after eating.
- Postnasal drip: Excessive mucus production due to allergies or sinus infections can trickle down the throat, causing coughing.
- Medication Side Effects: Certain medications, notably ACE inhibitors (e.g., Ramipril) used for blood pressure, can induce chronic coughing as a side effect.
- Chronic bronchitis or COPD: Persistent cough can be a hallmark of chronic lung conditions like bronchitis or chronic obstructive pulmonary disease (COPD).
- Smoking: A leading cause of chronic cough, smoking irritates the airways, leading to ongoing coughing spells.
Diagnostic approach and evaluation
Identifying the underlying cause of a prolonged cough involves a systematic approach.
1. Medical history and physical examination
- Your healthcare provider will inquire about the duration, nature, and triggers of the cough (e.g., cough that only occurs with certain allergic exposures or exercise in cold air, as in asthma). A physical exam may reveal clues about potential causes.
- The physical examination seeks clues suggesting the presence of cardiopulmonary disease, including findings such as wheezing or crackles on chest examination.
- Examination of the auditory canals and tympanic membranes (for irritation of the latter resulting in stimulation of Arnold’s nerve), the nasal passageways (for rhinitis or polyps), and the nails (for clubbing) may also provide aetiologic clues. Because cough can be a manifestation of a systemic disease such as sarcoidosis or vasculitis, a thorough general examination is likewise important.
2. Imaging tests
- Chest X-rays or CT scans help assess the condition of the lungs, detecting infections, masses, or structural abnormalities.
- In virtually all instances, evaluation of chronic cough merits a chest radiograph. The list of diseases that can cause persistent cough without other symptoms and without detectable abnormalities on physical examination is long.
- It includes serious illnesses such as sarcoidosis or Hodgkin’s disease in young adults, lung cancer in older patients, and (worldwide) pulmonary tuberculosis. An abnormal chest film prompts an evaluation aimed at explaining the radiographic abnormality.
3. Labs and cultures
- Blood tests, sputum cultures, or allergy tests might be conducted to identify infections or allergic triggers.
- In a patient with chronic productive cough, examination of expectorated sputum is warranted, because determining the cause of mucus hypersecretion is a crucial clue to aetiology.
- Purulent-appearing sputum should be sent for routine bacterial culture and, in certain circumstances, mycobacterial culture as well. Cytologic examination of mucoid sputum may be useful to assess for malignancy and oropharyngeal aspiration and to distinguish neutrophilic from eosinophilic bronchitis.
- Expectoration of blood whether streaks of blood, blood mixed with airway secretions, or pure blood deserves a special approach to assessment and management.
4. Pulmonary function tests: Assess lung function, vital for diagnosing conditions like asthma or COPD.
5. Bronchoscopy: Invasive but often necessary to examine the airways directly, especially if other tests are inconclusive.
6. Trial treatments: Sometimes, a healthcare provider might suggest a therapeutic trial to observe if treatments for specific conditions alleviate the cough.
Treatment
- Empiric treatment of chronic idiopathic cough with inhaled corticosteroids inhaled anticholinergic bronchodilators, and macrolide antibiotics has been tried without consistent success.
- Currently, available cough suppressants are only modestly effective. Most potent are narcotic cough suppressants, such as codeine, hydrocodone, or morphine, which are thought to act in the “cough centre” in the brainstem. The tendency of narcotic cough suppressants to cause drowsiness and constipation and their potential for addictive dependence limit their appeal for long-term use.
- Dextromethorphan is an over-the-counter, centrally-acting cough suppressant with fewer side effects and less efficacy than narcotic cough suppressants. Dextromethorphan is thought to have a different site of action than narcotic cough suppressants and can be used in combination with them if necessary.
- Benzonatate is thought to inhibit the neural activity of sensory nerves in the cough-reflex pathway. It is generally free of side effects; however, its effectiveness in suppressing cough is variable and unpredictable.
- Inhaled lidocaine, an inhibitor of voltage-gated sodium channels, provides transient cough suppression, but because of associated oropharyngeal anaesthesia, it poses the risk of aspiration.
- Attempts to treat cough hypersensitivity syndrome have focused on the inhibition of neural pathways. Small case series and randomised clinical trials have indicated benefit from off-label use of gabapentin, pregabalin, or amitriptyline. Recent studies suggest a role for behavioural modification using specialised speech therapy techniques, but widespread application of this modality is currently not practical. Novel cough suppressants without the limitations of currently available agents are greatly needed. Approaches that are being explored include the development of neurokinin-1 receptor antagonists, transient receptor protein vanilloid-1 (TRPV1) channel antagonists, a promising P2X3 channel antagonist (gefapixant), and novel opioid and opioid-like receptor agonists.
Clinical case
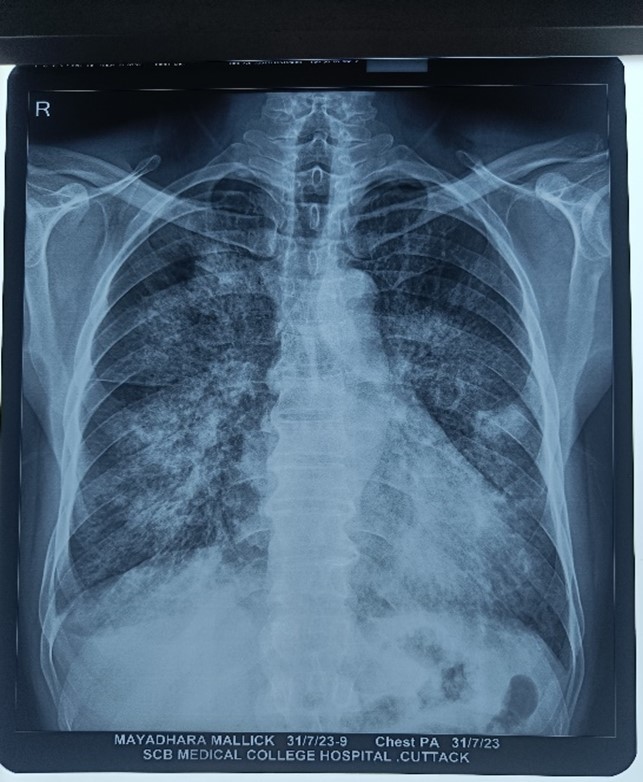
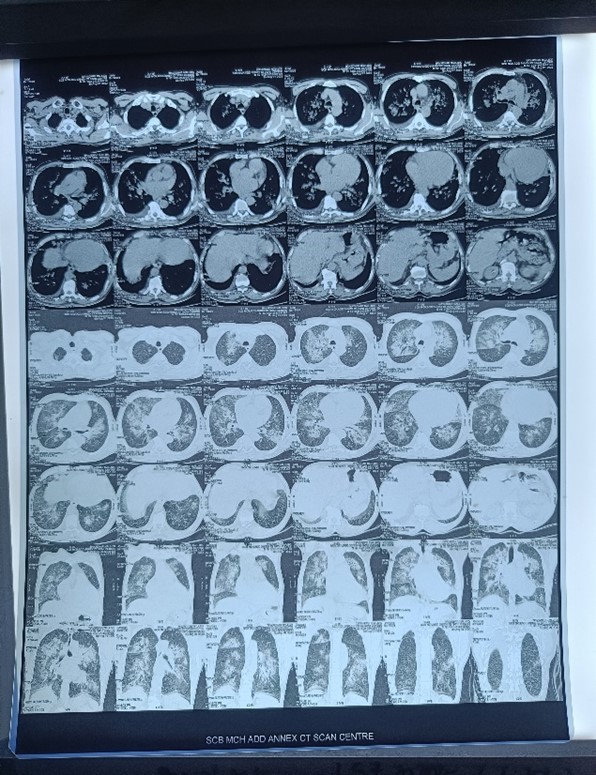
A 42-year-old male known diabetic presented to OPD with complaints of cough with scanty expectoration for 1.5 months (subacute) and shortness of breath for 15 days with a history of fever 1.5 months back subsided but now again high-grade fever for 6 days and chest pain. The patient was admitted to the hospital.
On auscultation, there was b/l coarse crepitations heard, and there was occasional Ronchi as well.
On investigations
- CBC- TLC was raised
- Chest x ray-right upper middle and lower zone haziness and left middle zone haziness
- HRCT-b/l ground glass opacities with bilateral lower lobe and right middle lobe consolidation with atelectasis (Infective aetiology)
- Sputum C/S- klebsiella pneumonia sensitive to tigecycline
A patient was started on tigecycline 50 mg IV BD and other symptomatic treatments. The patient improved clinically and symptomatically after 4 days.
Conclusion
Distinguishing between acute, subacute, and chronic coughs aids in understanding their potential causes and guiding appropriate evaluation and treatment. If you're experiencing a persistent cough, seeking medical attention is crucial for accurate diagnosis and management. A comprehensive evaluation ensures effective resolution, alleviating discomfort and addressing any underlying health concerns.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries