Stratification of ASCVD risk in cancer survivors: New guidelines
M3 India Newsdesk Jun 30, 2021
Cancer survivors have a higher risk of developing cardiovascular diseases as compared to the general population owing to the number of treatments that they go through to survive the disease, many at times developing ASCVD that can further complicate their health status. This article presents the recommendations for screening and management of the ASCVD risks in cancer patients with implications for India.
Snapshots
- Adult cancer survivors are at an increased risk of atherosclerotic cardiovascular disease (ASCVD), which is caused by conventional risk factors as well as cancer therapy.
- Due to a lack of evidence-based guidelines for optimal screening and care in this specific group, standard approaches may not accurately predict ASCVD risk in adult cancer survivors.
- More research is needed to verify the use of multimodal imaging and primary preventive therapy in this patient population.
What is atherosclerotic cardiovascular disease?
ASCVD is the second leading cause of mortality in this cancer population, after cancer. Obesity, diabetes, hypertension, hyperlipidaemia, cigarette use, poor nutrition, physical inactivity, and advanced age all contribute to the increased prevalence of ASCVD in adult cancer survivors. In the United States, the prevalence of pre-existing coronary artery disease (CAD) in oncology patients is estimated to range from 5.7 per cent (breast) to 20.8 per cent (lung). This association is influenced by treatment and malignancy-related variables. In individuals with clonal hematopoiesis of uncertain potential, for example, the risk of coronary artery disease is doubled. Childhood cancer survivors have a two- to twelve-fold increased risk of myocardial infarction when compared to their siblings, depending on the kind of cancer. Despite this, research indicates that ASCVD is underdiagnosed and undertreated among cancer survivors.
Cancer treatment and the risk of ASCVD
- Chemotherapeutics and radiation treatment have cardiotoxic effects, which increase the risk of ASCVD.
- Chest irradiation and chemotherapeutic medicines like platinum, anti-metabolites, VEGF inhibitors, and tyrosine kinase inhibitors (nilotinib) have all been related to hastening atherosclerosis and CAD. VEGF inhibitors can increase the risk of ASCVD by causing hypertension.
- Platinum treatment (cisplatin) causes procoagulant and endothelial damage, resulting in an 8% absolute risk of coronary artery disease over 20 years.
- Immune checkpoint inhibitors have been linked to a threefold increase in ASCVD events caused by accelerated atherosclerosis. Despite methods to reduce total radiation dosage, these individuals continue to have an increased risk of CAD in the future due to endothelial damage, thrombosis, and plaque rupture.
- Antimetabolites (fluorouracil, capecitabine) cause vasospasm and endothelial damage, resulting in ischaemia.
- Androgen deprivation treatment leads to dyslipidaemia and insulin resistance, both of which are known risk factors for ASCVD.
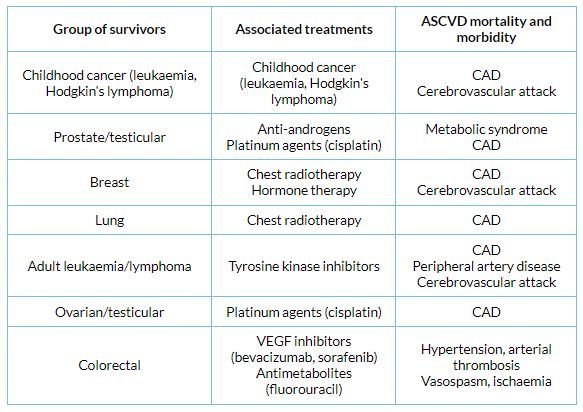
Association of oncologic treatment with the development of adverse cardiac events
Stratification of ASCVD risk
- The increased risk of ASCVD events among cancer survivors is not captured by traditional risk classification techniques. Although some guidance has been offered, the function of primary prevention of ASCVD in cancer survivors is also unknown.
- Prior to and after starting targeted cancer therapy, the Canadian Society of Cardiology highlights the need of following established risk-stratification guidelines.
- Hodgkin's disease and testicular tumours are high-risk tumours for CAD, according to the American Society of Oncology, although there is little research on primary prevention in these individuals.
- The European Society of Cardiology's consensus panel advocates assessing conventional risk factors before starting cancer treatment, screening specific groups (e.g., those using fluoropyrimidines) using electrocardiography, and testing for the existence of CAD if necessary.
- The Cardiovascular Risk Calculator from the Childhood Cancer Survivor Study can also be used by individuals over the age of 50 who have had treatment for childhood cancer.
- When estimating a patient's 10-year risk for ASCVD, Jurado et al. advocate using mediastinal radiation as a risk-enhancing factor alongside smoking.
- The American Heart Association (AHA) presents a simple yet proven approach for patient counselling in the lack of substantial, high-quality data for the prevention of CAD in cancer patients. Smoking cessation, regular exercise, and avoiding metabolic syndrome are all important factors in lowering cardiovascular risk.
Recommendations for screening and other risk stratification tools
Several societies have issued consensus statements concerning when and how to test for CAD, despite the fact that there are no recommendations for risk stratification of cancer patients for ASCVD prevention. To determine the necessity for structural or functional imaging, the Society for Cardiovascular Angiography and Intervention suggests an annual review of risk factors, as well as history and clinical exam. This includes a thorough examination for CAD symptoms as well as a physical examination. Assessment with coronary computed tomography angiography (CCTA) or non-invasive stress testing every 5 years is recommended in individuals who had chemotherapy that provides a persistent vasotoxic risk (e.g., nilotinib, ponatinib, and cisplatin). Patients who got chest radiation owing to the possibility of silent ischaemia are given similar advice. Expert panels on monitoring for radiation-associated heart disease have been issued by the American College of Cardiology (ACC), the American Society of Echocardiography (ASE), and the European Association of Cardiovascular Imaging (EACVI).
The ACC/ASE/EACVI, for example, recommends screening echocardiography 10 years after therapy and then every 5 years after that. They recommend screening at 5 years after treatment and non-invasive stress testing every 5 years for individuals at high risk for radiation-induced cardiac disease. Stress echocardiography and cardiac magnetic resonance imaging are recommended screening modalities due to their better specificity; nevertheless, if these investigations are equivocal, cardiac computed tomography might be investigated.
Observational studies indicate that screening for coronary artery disease using CCTA may be beneficial. Nevertheless, the optimal time of imaging remains unknown. Furthermore, existing evidence shows that coronary artery calcium (CAC) scoring may aid in risk stratification of radiation or chemotherapy patients. When CAC = 0, patient fatalities in the CAC consortium were more frequently related to malignancy. When the CAC score was more than 300, ASCVD was the leading cause of mortality.
As it is a common procedure for ischaemia assessments, other imaging modalities like cardiac magnetic resonance imaging, fluorodeoxyglucose positron emission tomography, and single-photon emission computed tomography can be used on oncology patients.
Managing the risk of ASCVD in cancer survivors
There is no information on using statins as primary prevention in adult cancer survivors. Present suggestions are to follow current society guidelines, such as starting statin medication in oncologic patients with a high 10-year risk of ASCVD events. Non-statin therapies, such as ezetimibe or PCSK9 inhibitors, may be used in patients with particularly high-risk profiles and insufficient reduction of low-density lipoprotein cholesterol; diet, lifestyle, and physical activity counselling, as well as management of comorbid conditions such as hypertension, obesity, and diabetes, should occur concurrently.
Implications for India
Cancer mortality in India has more than doubled since 1990. India's cancer incidence is anticipated to have increased by 1.15 million new patients in 2018 and is expected to almost quadruple by 2040 due to demographic trends alone. In urban and rural India, respectively, cancer is the second and fourth major cause of adult death. Cancer has surpassed heart disease as the primary source of catastrophic health cost, distress finance, and growing cost before death in India. ASCVD risk among cancer patients has been an underrated problem that needs due attention.
Effective measures are required to reduce the risk of ASCVD in cancer survivors. There are no prospective trials validating conventional ASCVD screening techniques or the implications of initiating primary preventive treatment in this cohort. A rising amount of data supports cancer's inclusion as a risk factor. Numerous societies promote multimodal imaging, however, the incorporation of CAC and CCTA into risk stratification for oncologic patients requires more investigation. In the absence of these data, the AHA's Life's Simple 7 is a very useful clinical tool for lowering the risk of ASCVD. Providing treatment to cancer patients is difficult, given the underlying conventional cardiac risk factors and the shifting nature of cancer therapy. As such, it is probable that a multidisciplinary survival team will be required to offer complete cardiac care.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries