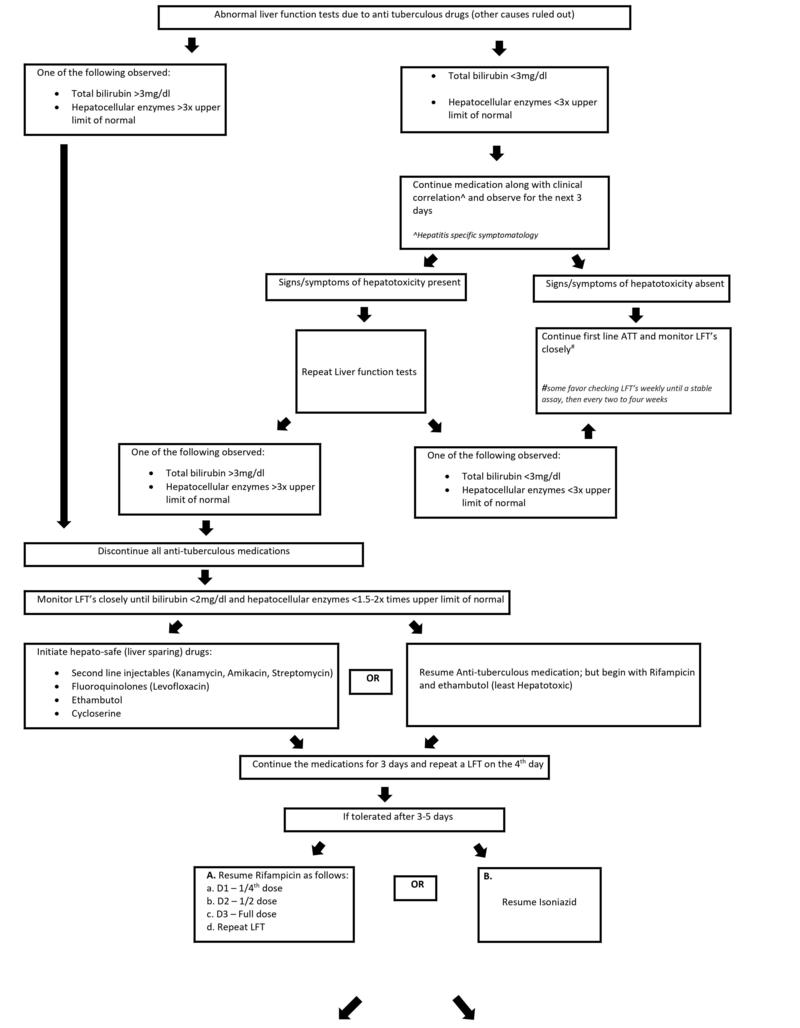
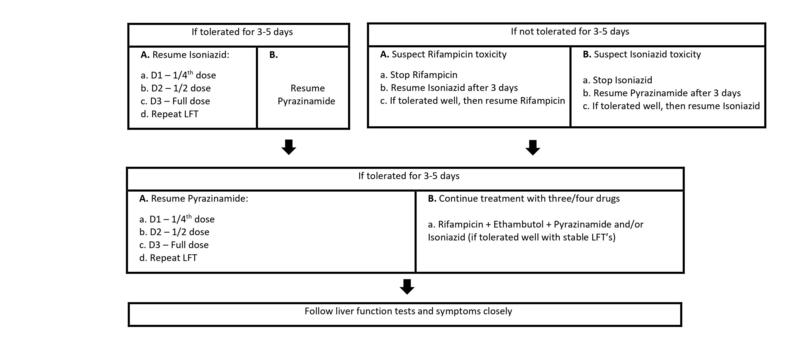
Step-wise protocol for anti-tuberculous treatment-induced hepatitis
M3 India Newsdesk Jun 22, 2021
Patients diagnosed with TB have to be administered medications that may contribute to hepatotoxicity. This article discusses the line of treatment and drug protocol followed for drug-induced hepatitis in hospitals.
Introduction
The global management of tuberculosis comprises isoniazid(H), rifampicin(R), ethambutol(E) and pyrazinamide (Z) for an intensive phase of 2 months followed by a 4-month period of a continuation phase. One of the most common adverse effects of anti-tuberculous treatment (ATT) is drug-induced hepatitis which has a mortality rate of 5%. However, despite the low mortality rate, adverse symptomatology is one of the reasons for poor compliance and altered adherence pattern.
Medication
The drugs known to cause hepatotoxicity are pyrazinamide, isoniazid, and rifampicin (in decreasing order of frequency). Given below is a series of protocols followed for drug-induced hepatitis management in a government hospital.
After clinical + microbiological / radiological confirmation of active tuberculosis
↓
A pre-test evaluation is done to rule out other discrete pathologies
- Liver function tests*
- Renal function tests
- HIV/ HbsAg
- Complete blood count
* LFT’s include: Aminotransferases, serum bilirubin, alkaline phosphatases
Liver function tests
The LFTs are done usually at the start of the treatment as mentioned above and if normal, they are hardly ever repeated. However, for some clinicians, timely monitoring of LFTs while on treatment is preferred. This is carried out along with appropriate counselling to avoid the use of alcohol and drugs associated with hepatotoxicity (such as acetaminophen). Risk factors for drug-induced liver injury including underlying liver disease (particularly hepatitis C) and coadministration of antiretroviral therapy for patients with HIV infection need to be ruled out.
Elevations in liver aminotransferases (ALT/AST) are usually seen in the first 3 weeks of treatment initiation and the symptoms we see are:
- Vomiting (at first: right after taking the medication; followed by untimely random bouts of excessive vomiting)
- Abdominal pain
- Infrequent febrile episodes
- Jaundice
- Anorexia
Antituberculosis drugs
A general dictum on discontinuing all the antituberculosis drugs- If the serum bilirubin is ≥3 mg/dL or serum transaminases are more than 5 times the upper limit of normal. If the condition of the patient deteriorates from TB, then the treatment cannot be stopped. The patient is given streptomycin and ethambutol until the liver transaminases return to normal (these two drugs are not associated with hepatitis). Fulminant hepatitis can occur in the course of TB treatment but is fortunately rare; emergency liver transplantation may be necessary, and deaths do occur.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries