Recognition and Management of Sepsis and Septic Shock
M3 India Newsdesk Mar 19, 2024
Sepsis and septic shock present a growing global health concern, with a high mortality rate. Early recognition, prompt antibiotic therapy, and targeted management strategies, including fluid resuscitation and source control, are crucial in improving patient outcomes and reducing mortality.
Since the initial consensus definition of sepsis (Sepsis-1) in 1991, there has been a consistent rise in the occurrence of both sepsis and septic shock. By 2017, the global tally stood at approximately 49 million cases of sepsis, resulting in around 11 million deaths attributed to sepsis-related complications.
Globally, the population incidence of hospital-treated sepsis in adults is estimated at 270 per 100,000. Without counting sepsis in children or occurring outside hospitals, this equates to 19.4 million cases and 5.3 million deaths globally each year.
The World Health Organisation (WHO) designated it as a top priority in global health.This staggering increase in incidence can be attributed to different factors:
- The advanced average age among patients
- The increased number of invasive procedures
- The wide usage of immunosuppressive drugs and chemotherapy
- Antibiotic resistance
In addition, septic patients have a high risk of in-hospital mortality (IHM), accounting for approximately 20% of all-cause deaths globally, rendering this combined ailment one of the highest mortality conditions encountered in the emergency department (ED).
Definition of sepsis and septic shock
The Third International Consensus Definitions for Sepsis and Septic Shock were released in February 2016.
Sepsis is now defined as ‘life-threatening organ dysfunction caused by dysregulated host response to infection’.
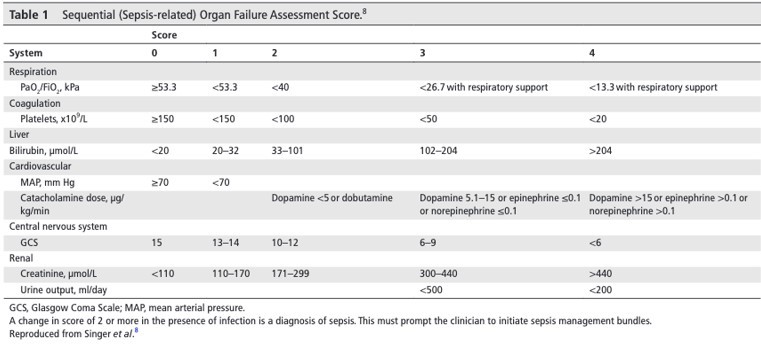
Aberrant regulation of normal physiological responses to infection, encompassing both pro-inflammatory and anti-inflammatory reactions, can lead to severe organ dysfunction. The clinical diagnosis of sepsis relies on the presence of infection in a patient and an elevated Sequential (Sepsis-related) Organ Failure Assessment Score (SOFA), with a change in score of 2 or more from baseline being indicative (table below).
Septic shock is characterised as a subgroup of sepsis marked by severe circulatory, cellular, and metabolic dysfunctions, posing a higher mortality risk compared to sepsis alone. The criteria for diagnosing septic shock include the need for vasopressors to maintain a mean arterial pressure (MAP) above 65 mm Hg, along with a serum lactate level exceeding 2 mmol/L in the absence of hypovolemia. This updated definition of septic shock aims to identify patients with an in-hospital mortality rate exceeding 40%.
Risk factors for developing sepsis
Sepsis arises from the body's reaction to infection, making the most vulnerable populations include infants, the elderly, individuals with weakened immune systems, and those with underlying health conditions such as diabetes or cancer.
Recognition of sepsis
The timely identification and resuscitation of septic patients are vital for managing sepsis effectively. Consequently, individuals showing signs of deterioration and presenting with an elevated early warning score (e.g., an aggregate early warning score of 5 or higher) should be assessed for potential infection.
Systemic inflammatory response syndrome and sepsis
Systemic inflammatory response syndrome (SIRS) denotes a pro-inflammatory condition that may not always be triggered by infection. To meet the criteria for systemic inflammatory response syndrome (SIRS), a patient must have two or more of the following:
- Temperature >38°C or <36°C
- Respiratory rate >20 breaths per minute
- Heart rate >90 beats per minute
- White blood cell count of >12×109 /L or <4×109 /L SIRS criteria should prompt assessment for sepsis and septic shock and apply initial management although it's no longer required for the diagnosis of sepsis.
Early recognition
Many clinicians utilise track-and-trigger early warning score systems as a standard approach to identify patients at risk of deterioration. Two such examples are the National Early Warning Score (NEWS) and the Modified Early Warning Score (MEWS), commonly utilised in the UK (table below).
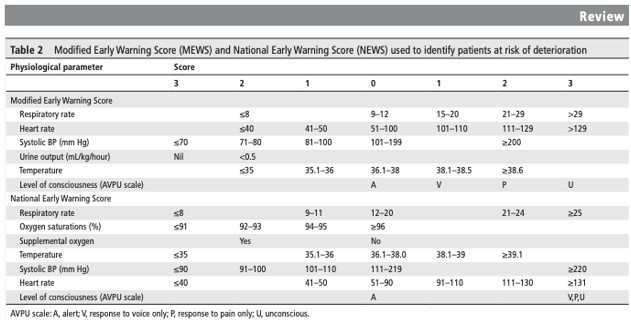
These scores are validated tools for predicting adverse outcomes and are widely utilised in healthcare settings. Front-line clinicians should adhere to the tool recommended by their institution or local sepsis teams to detect inflammatory responses in sepsis.
Investigations
When caring for a patient with sepsis, it is essential to conduct initial evaluations to recognise indications of end-organ hypoperfusion and ascertain the origin of infection. Investigations aimed at assessing for end-organ hypoperfusion include:
- Full blood count
- Clotting profile, with prothrombin time and INR
- Urea and electrolytes
- Liver function tests
- Serum lactate
- Arterial blood gas measurement
Management strategies
The management protocol (depicted below) delineates the fundamental strategies for addressing and preventing the life-threatening complications linked with sepsis and septic shock.
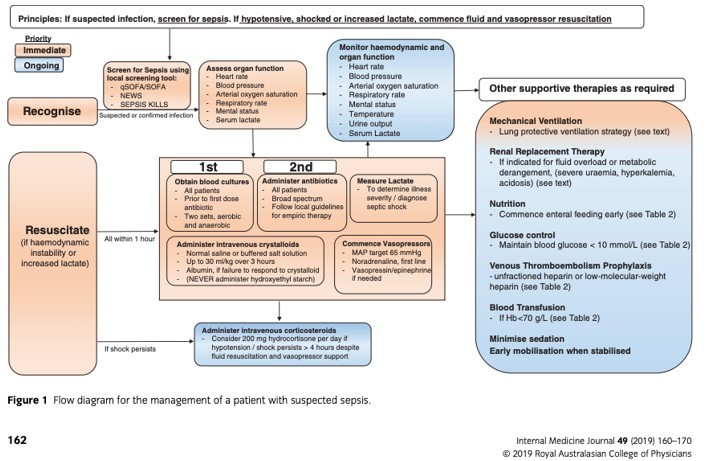
Antibiotics: Early antibiotic therapy and the recommendation has been supported by compelling evidence.
The 2016 updated guidelines of the Surviving Sepsis Campaign, endorsed by the European Society of Critical Care Medicine, the International Sepsis Forum, and the Society of Critical Care Medicine, advocate for the administration of intravenous antibiotics within one hour of sepsis recognition. A significant retrospective study analysing Surviving Sepsis Campaign data in 2014 validated that any delay in administering antibiotics correlates with higher in-hospital mortality rates, with a proportional rise in mortality risk for every hour of delay.
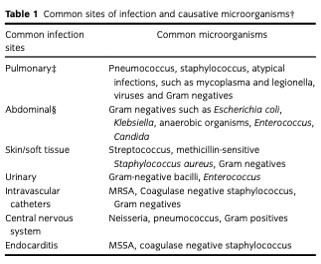
The empiric choice of antimicrobials may need to cover resistant organisms such as Methicillin-resistant Staphylococcus aureus, Vancomycin-resistant enterococci, Gram-negative bacteria, particularly Klebsiella pneumonia and Escherichia coli.
Intravenous fluids: For initial fluid resuscitation, it is recommended to use crystalloid solutions due to concerns regarding colloid solutions potentially increasing the risk of acute kidney injury. In patients exhibiting hypoperfusion, an intravenous crystalloid fluid challenge of at least 30 mL/kg should be administered within three hours. Monitoring the response to fluids is crucial to avoid fluid overload or exacerbation of sepsis-induced acute lung injury.
Source control: Actions aimed at eradicating the source of infection, managing ongoing contamination, and restoring the body's normal anatomy and function are essential. According to Surviving Sepsis Campaign guidelines, these interventions should occur within the initial 12 hours following diagnosis, prioritising the use of minimally invasive procedures. These measures may involve draining infected fluid collections, debriding infected tissue, and removing devices and foreign bodies such as intravascular access devices or performing surgical interventions.
Monitoring response to treatment: Traditionally, therapy has been used to mean intensive-care-based protocoled management to meet the following physiological targets:
- Mean arterial pressure of 65mm Hg.
- Urine output of 0.5mL/kg/hour.
- Central venous pressure of 8–12mm Hg.
- Superior vena cava oxygen saturation of 70% or mixed venous oxygen saturation of 65%.
- The 2016 updated Surviving Sepsis Campaign guideline underscores the advantages of promptly identifying and resuscitating patients with sepsis and septic shock. If intravenous fluid targets are not achieved, it is recommended to promptly refer the patient to critical care services.
Vasopressors and Inotropes: For patients who maintain hypotension despite receiving sufficient fluid resuscitation or develop cardiogenic pulmonary oedema, the use of vasopressors is warranted. In cases of myocardial dysfunction or failure to achieve adequate end-organ perfusion despite sufficient intravascular fluid volume and maintaining mean arterial pressure (MAP), inotropes may be considered for initiation.
Norepinephrine is the primary vasopressor of choice for patients requiring such treatment. Vasopressin or epinephrine may be adjunctively administered if necessary. In cases where patients continue to exhibit instability, dobutamine is recommended.
Corticosteroids: Hydrocortisone is considered adjunctive therapy for patients with septic shock who do not attain sufficient mean arterial pressure (MAP) despite receiving appropriate intravenous fluid and vasopressor support.
Transfusion of blood products: Patients diagnosed with sepsis should undergo red blood cell transfusion when their haemoglobin levels drop below <7 g/dL.
Glucose control: The Surviving Sepsis Campaign recommends implementing an insulin protocol to keep glucose levels below 10 mmol/L in sepsis, aiming to prevent hypoglycemia and abrupt glucose fluctuations. Serum glucose levels should be monitored every 1 to 2 hours until they stabilise, and then every 4 hours thereafter.
Airway support and oxygen: Ensuring airway stability is crucial, especially in patients with reduced consciousness levels, to maintain sufficient tissue oxygenation and sustain oxygen saturation above 94%.
Additional care: Prophylaxis for venous thromboembolism (VTE), stress ulcers, and pressure ulcers.

Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Akshayaa is a General Practitioner at Sri. Balaji Heart Centre, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries