Peptic Ulcer Management
M3 India Newsdesk Dec 18, 2023
This comprehensive article illuminates Peptic Ulcer Disease (PUD), delineating its effective management and improved patient outcomes. Along with empowering informed decision-making for optimal patient care and well-being.
Case study
A 45-year-old male with a medical history of no significant prior medical conditions except occasional heartburn and indigestion was presented to the clinic. He complained of recurrent episodes of gnawing abdominal pain. He described the pain as a burning sensation in the upper abdomen, often occurring between meals and sometimes waking him up at night.
He mentioned that the pain seemed to subside temporarily after eating or taking over-the-counter antacids. Additionally, he experienced occasional heartburn, bloating, and a feeling of nausea, but no vomiting. The patient admitted to experiencing weight loss recently but attributed it to stress and a busy work schedule.
Assessment and diagnosis
Upon physical examination, no acute abnormalities were noted. However, based on the patient's symptoms, the physician suspected Peptic Ulcer Disease (PUD). To confirm the diagnosis and identify potential causes, the following diagnostic tests were conducted:
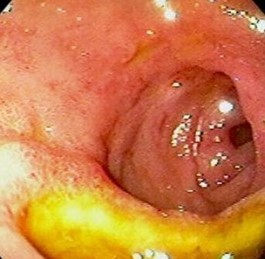
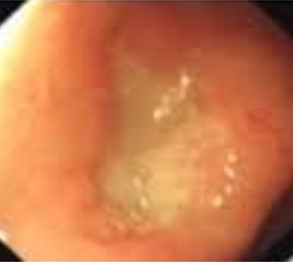
Endoscopy: An upper endoscopy revealed the presence of an ulcer in the duodenal region, confirming the diagnosis of peptic ulcer disease.
H. pylori testing: Blood tests were conducted to detect the presence of H. pylori bacteria, which came back positive, suggesting an H. pylori infection as one of the underlying causes of the ulcer.
Treatment plan
Based on the diagnosis, the patient's treatment plan was devised, considering the H. pylori infection and the ulcer:
Medication
The physician prescribed a course of antibiotics (clarithromycin, amoxicillin) along with proton pump inhibitors (PPIs) to eradicate the H. pylori infection and reduce stomach acid production, aiding ulcer healing.
Lifestyle modification
The patient was advised to abstain from NSAIDs, quit smoking, moderate alcohol intake, and opt for smaller, more frequent meals.
Follow-up: Regular follow-up appointments were scheduled to monitor the progress of treatment and ensure the ulcer was healing properly.
Outcome
Following the prescribed treatment regimen, the patient reported a significant reduction in abdominal pain within a few weeks. A follow-up endoscopy revealed a notable improvement in the ulcer's appearance, indicating successful healing. Furthermore, H. pylori testing post-treatment indicated the eradication of the bacterial infection.
Conclusion
The patient's case demonstrates the importance of early diagnosis and targeted treatment in managing Peptic Ulcer Disease. Proper medication, lifestyle modifications, and regular monitoring led to the successful healing of the ulcer and eradication of the underlying H. pylori infection, ensuring the patient's overall health and well-being.
What is peptic ulcer disease?
- Peptic ulcer disease refers to the development of painful ulcers in the stomach lining or the initial segment of the small intestine known as the duodenum. Normally, the stomach's lining is shielded by a thick layer of mucus that guards against the harmful effects of its digestive juices. However, factors that compromise this protective layer can allow stomach acid to harm the tissue, resulting in ulcers.
- Certain individuals have a higher susceptibility to ulcers, with approximately one in ten people experiencing this condition.
Various risk factors contribute to an increased likelihood of developing ulcers, including:
- Regular use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, commonly used for pain relief
- A familial history associated with ulcers
- Presence of specific illnesses such as liver, kidney, or lung diseases
- Consistent consumption of alcohol
- Smoking habits
Previous beliefs attributing stress or certain foods as direct causes of ulcers have been debunked by research.
Instead, studies have identified two primary causes responsible for the development of ulcers:
Helicobacter pylori (H. pylori) bacteria: This bacterial infection typically affects the stomach, triggering inflammation that weakens the protective mucus layer. As a result, the stomach lining becomes susceptible to damage by stomach acid, leading to ulcer formation.
Pain-relieving NSAID medications: Continuous use of NSAIDs like aspirin and ibuprofen can erode the protective mucus layer in the digestive tract, rendering the stomach lining more vulnerable to damage and ulcers.
H. pylori bacteria
- H. pylori infection is widespread, affecting roughly 50% of the global population, often without noticeable symptoms. Transmission commonly occurs from person to person, particularly during childhood.
- These bacteria adhere to the mucus layer in the digestive tract, leading to inflammation that compromises the protective lining. Consequently, the stomach's robust acidic environment intended for food digestion can harm the stomach tissue in the absence of this protective layer.
- Although most individuals with H. pylori don't experience negative effects, only a smaller subset, approximately 10% to 15%, develop ulcers.
Pain relievers
- NSAIDs, a class of medications utilised for pain relief, constitute a significant cause of peptic ulcer disease. These drugs can gradually erode the protective mucus layer in the digestive tract, potentially leading to the formation of peptic ulcers.
- Common NSAIDs like aspirin, naproxen, and ibuprofen, including prescription variants, pose risks. However, acetaminophen, not categorised as an NSAID, does not inflict damage on the stomach. Consequently, individuals unable to take NSAIDs are often advised to consider acetaminophen.
- While not everyone using NSAIDs develops ulcers, combining NSAID use with an H. pylori infection heightens the risk significantly. Individuals with both factors are more susceptible to severe damage to the mucus layer, potentially leading to more severe consequences.
Other causes
- Peptic ulcer disease can also arise from less frequent circumstances, including severe illness due to various infections or diseases, post-surgery complications, or the intake of certain medications like steroids.
- Rarely, a condition known as Zollinger-Ellison syndrome (gastrinoma) can cause peptic ulcers. This syndrome involves the formation of tumours comprising acid-producing cells in the digestive tract. These tumours, whether cancerous or noncancerous, generate excessive acid that damages the stomach tissue.
Influence of coffee and spicy foods on ulcers
Contrary to popular belief, there's a common misconception that attributes the cause of ulcers to coffee and spicy foods. Previously, the notion prevailed that individuals with ulcers should adhere to a bland diet. However, current understanding indicates that individuals with ulcers can consume a variety of foods, provided these choices do not exacerbate their symptoms.
Symptoms of ulcers
Some individuals afflicted with ulcers may not manifest any symptoms. However, indicative signs of an ulcer might encompass:
- Gnawing or burning pain in the middle or upper stomach, occurring between meals or during the night
- Pain that subsides temporarily upon consuming food or utilising antacids
- Feelings of bloating
- Occasional heartburn
- Episodes of nausea or vomiting
Severe symptoms
In more severe instances, individuals may experience heightened manifestations such as:
- Dark or black stool, suggestive of bleeding
- Frequent episodes of vomiting
- Unexplained weight loss
- Severe and persistent pain in the mid to upper abdomen
These symptoms, especially the severe ones, warrant prompt medical attention and evaluation for appropriate diagnosis and treatment of ulcers.
Diagnosis and testing for ulcers
- Symptom assessment: Healthcare providers often begin diagnosing ulcers by discussing and evaluating the patient's symptoms. In cases where NSAIDs are not in use, an H. pylori infection is a probable cause.
- Endoscopy: For severe symptoms or to confirm ulcer presence, an upper endoscopy might be recommended. This procedure involves inserting an endoscope (a small, illuminated tube housing a camera) through the throat to examine the stomach for abnormalities.
- H. Pylori tests: Widely used tests for H. pylori infection help in tailoring treatment. These tests include:
- Breath test: A straightforward method to detect H. pylori.
- Blood or stool test: Alternative methods for detecting H. pylori infection.
- Sample collection during endoscopy: A direct sampling method during an upper endoscopy procedure.
- Imaging tests: Less frequently utilised, imaging tests like X-rays or CT scans can be employed to identify ulcers. These tests may involve drinking a specific liquid that enhances the visibility of ulcers within the digestive tract for imaging machines.
These diagnostic methods assist healthcare providers in confirming the presence of ulcers, identifying potential causes such as H. pylori infection, and subsequently tailoring treatment strategies to manage symptoms and eradicate the underlying causes.
Management and treatment of ulcers
- Natural healing: In some cases, ulcers may naturally heal without intervention. However, it's crucial not to disregard warning signs. Untreated ulcers can lead to severe health complications such as bleeding, perforation, or gastric outlet obstruction due to swelling or scarring that blocks the passage from the stomach to the small intestine.
- Medical interventions: When ulcers require treatment, various options exist:
- Bleeding ulcer procedures: Doctors might perform endoscopy to administer medications, use clamps, or employ cauterisation to stop bleeding in bleeding ulcers.
- Medications: Commonly prescribed drugs include proton pump inhibitors (PPIs), histamine receptor blockers (H2 blockers), antibiotics (for H. pylori), and protective medications that act as a barrier to shield ulcers from digestive acids and enzymes.
Prevention
- Alternatives to NSAIDs: Discuss alternative pain relief options (such as acetaminophen) with your doctor.
- Protective measures: If you cannot cease NSAID usage, discuss protective measures with your healthcare provider.
- NSAID dosage and timing: Opt for the lowest effective NSAID dose and take it with a meal.
- Lifestyle changes: Quit smoking, and if you consume alcohol, do so moderately or consider abstaining.
Outlook and prognosis
Curability: Treatment targeting the root cause, often H. pylori bacterial infection or NSAID use, effectively eliminates peptic ulcer disease for most individuals. However, there is a risk of ulcer recurrence, especially if H. pylori is not entirely eradicated from your system or if you continue smoking or using NSAIDs.
Following these preventive measures, adhering to prescribed treatments, and making necessary lifestyle modifications can significantly reduce the likelihood of developing or experiencing recurrent ulcers, contributing to a better prognosis and improved overall health. Regular consultations with healthcare professionals can aid in managing ulcers effectively.
Healing duration of ulcers
Typically, it takes several weeks of consistent treatment for an ulcer to heal properly.
Living with ulcers
- Milk's role: While milk might briefly alleviate ulcer pain due to its coating effect on the stomach lining, it can also prompt increased stomach acid and digestive juices, potentially worsening ulcers over time.
- Safety of antacids: Antacids provide temporary relief from ulcer symptoms but may interfere with the efficacy of prescribed medications. Consulting your doctor is advisable to determine the safety of using antacids alongside ongoing treatment.
- Dietary recommendations: No specific foods have been definitively proven to have a positive or negative impact on ulcers. However, maintaining a nutritious diet, regular exercise, and adequate sleep contribute positively to overall health.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Jimmy Patel is a practising gastroenterologist in Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries