Paediatric Febrile Seizures
M3 India Newsdesk May 03, 2023
A seizure is a transient occurrence of signs or symptoms resulting from abnormal excessive or synchronous neuronal activity in the brain. This article explains the pathophysiology, prognosis and management of paediatric febrile seizures.
Acute symptomatic seizures are secondary to an acute problem affecting brain excitability, such as electrolyte imbalance or infection. Epilepsy is defined as recurrent, unprovoked seizures.
Seizures in the setting of fever may be caused by either of the following:
- Central nervous system infections (meningitis, encephalitis, brain abscess)
- First presentation of epilepsy triggered by fever
- Febrile seizures
Febrile seizures
It represents the most common cause of seizures among children between 6 months and 5 years of age, occurring in about 4% of all children.
By definition, a febrile seizure occurs in the presence of a fever. It is defined as a seizure accompanied by a fever without central nervous system infection, metabolic or electrolyte disturbances, or a history of afebrile seizure or any acute neurological insult/head trauma in children aged 6 months to 6 years. Few guidelines include younger children up to 3 months
Simple febrile seizures are generalised at onset, last less than 15 minutes, and occur only once in a 24-hour period.
Complex febrile seizure occurs if the seizure has focal features, lasts longer than 15 minutes, or recurs within 24 hours and/or has incomplete recovery within 1 hour.
Febrile status epilepticus is the febrile seizure lasting for 30 minutes or more and/or a series of seizures without full recovery in between that.
Afebrile febrile seizures are seizures in an acute infectious illness (particularly gastroenteritis) without documented fever and feature consistent with simple FS.
Febrile seizure plus are seizures that continue past the usual age where they are expected to resolve (6 years) and/or are accompanied by afebrile, generalized or focal seizures.
Genetic Epilepsy with Febrile Seizure Plus- Febrile seizures plus with a family history of FSs, FSs plus, or afebrile generalised or focal seizures.
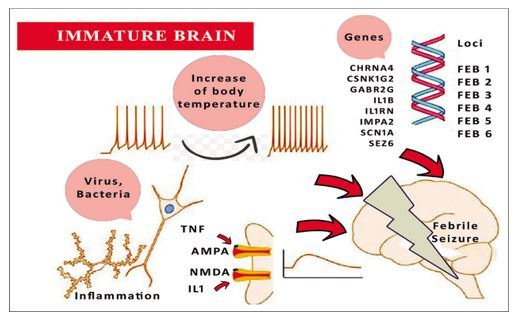
Pathophysiology
- In genetically predisposed children, an increase in brain temperature leads to perturbation of temperature-sensitive ion channels that in turn causes increased neuronal firing.
- Interleukin-1β acts as both a pyrogen and seizure provocateur, acting at the glutamate pathway. Interleukin-1β is also an NMDA agonist.
- Hyperthermia-induced brain alkalosis is also believed to result in neuronal excitability.
- Developing brain, especially those under 3 years have inherent increased vulnerability to neuronal excitation and low seizure threshold that explains high fever-related seizure burden in children.
Aetiology
- The most common infection is respiratory tract infection.
- The three most common viral isolates - the influenza virus, adenovirus, and parainfluenza virus. (ALSO tropical infections such as malaria and dengue).
- Various patterns of inheritance such as:
- Autosomal dominant inheritance with reduced penetrance
- Polygenic or multifactorial inheritance.
- FS may develop due to mutations in the gene that encodes for the γ-aminobutyric acid A receptor and sodium channels. This mutation depletes peak sodium current for a positive shift in the voltage-dependent activation when expressed in nonneuronal cells.
Investigations
|
Simple febrile seizure (SFS) |
Complex febrile seizure (CFS)/ febrile status epilepticus (FSE) |
|
|
Lumbar puncture |
Features of meningitis:
|
Children who remain obtunded after 1 hour of seizure |
| Neuroimaging |
Routinely not recommended. Consider either of the following; 1. Prior to lumbar puncture in children with focal neurological deficits. 2. Clinical symptoms and signs of raised intracranial pressure. |
1. MRI brain should be preferably considered within 72 hours(R/O viral encephalitis/SOL/Malformations/ Hippocampal ABN) 2. If the pre-existent developmental delay; a) Acute stage T2 hyperintensities after prolonged FS may lead to hippocampal sclerosis. However, whether this leads to temporal lobe epilepsy on follow-up remains to be seen. b) Also, the therapeutic implications of finding these abnormalities in acute-stage imaging are not clear at present. |
| EEG |
No |
Yes (>48 hrs ,<7 days after seizure) EEG may be useful in the acute setting if the child remains encephalopathic after the seizure and is not regaining the baseline status, primarily to rule out ongoing electrographic events. |
|
S. electr, Mg,RBS |
No | Yes |
| S. Ca |
If < 1 year |
Yes |
| S. Iron |
If clinical pallor |
If clinical pallor |
|
Urine r |
All children > 18 month, < 18 month if s/o UTI |
All children > 18 month, < 18 month if s/o UTI |
Genetic testing for Dravet syndrome (SCN1A, SCN1B, GABRG2, and SCN2A)
- Recurrent febrile status epilepticus
- The onset of prolonged hemiconvulsive seizures below 1 year of age
- Vaccine-associated encephalopathy
- GEFS+
Management
- Parental counselling is an important mainstay of treatment of febrile seizures, as they are by and large benign.
- Educate the family that even though dramatic in appearance, these seizures do not lead to neurological disease or dysfunction.
- Six hourly paracetamol may be advised for the first 48 hours in case of future episodes of fever. Antipyretic medications administered round the clock for the duration of fever may not prevent the occurrence or recurrence of seizures but will make the child less uncomfortable.
- Parents must be educated and trained in the home management of seizures and the use of abortive medication.
- Rescue seizure medication should be considered when the febrile seizure lasts longer than 3-5 minutes.
The drug of choice for rescue management
- At home is intra-nasal midazolam (0.2 mg/kg; maximum: 5 mg).
- Other effective drugs are intramuscular/buccal midazolam, buccal lorazepam, and per rectal diazepam.
- Maximum two doses, 5 minutes apart.
Management of febrile status epilepticus at the hospital
- This is similar to the management of convulsive status epilepticus. ; Stabilise with the ABCDE approach (airway, breathing, circulation, disability, and exposure/ examination).
- If diagnosed with Dravet syndrome, FS+, GEFS+, and sodium channel blockers (phenytoin) may be avoided.
- In young children, in case of clinical suspicion of meningitis and febrile status start third-generation cephalosporin till lumbar puncture results.
Prophylaxis
- Neither continuous nor intermittent anticonvulsant therapy is recommended for children with one or more simple FSs as there is a preponderance of harm over benefit with therapy.
- Intermittent prophylaxis with an oral benzodiazepine may be considered among children with;
- Frequent recurrent simple FSs with parental anxiety and residence far from medical facilities.
- Complex FS who have not been started on continuous prophylaxis. Drug of choice- Clobazam (0.5–1 mg/kg/day in two divided doses for 3 days without tapering; maximum dose 20 mg/day).
- Continous prophylaxis with anticonvulsants may be considered among children with;
- Febrile status epilepticus
- FSs in children with neurodevelopmental delays like cerebral palsy, global developmental delay or autism spectrum disorder.
- Frequent complex FSs
- Children with FS+/GEFS+ with afebrile seizures. Drug of choice - Sodium Valproate (20–40 mg/kg/ day), Phenobarbital (3–5 mg/kg/day); Primidone (15–20 mg/kg/day) (Carbamazepine and phenytoin are ineffective).
Future prognosis
A] Future risk of epilepsy
- Simple febrile seizures - 1% risk of developing epilepsy by the age of 7 years (same as the general population) and 2.4% by 25 years of age.
- Multiple simple febrile seizures /<1 year; family history of epilepsy:
- With 1 complex feature: 6–8%
- With 2 complex features: 17–22%
- With 3 and more features: 49%
- Risk factors for developing subsequent epilepsy:
- family history of epilepsy
- neurodevelopmental problems
- prolonged or focal febrile seizures
- febrile status epilepticus
B] Recurrence of febrile seizures
- 32% of children have recurrent seizures 17%- have one recurrence; 9%- have two recurrences; 6% have three or more recurrences.
- Recurrence rate within 1 year and 2 years of the first febrile seizure is 75% and 90%, respectively.
- Risk factors for recurrent febrile seizures:
- Early onset <18 months of age
- Family history of febrile seizures or epilepsy in a first-degree relative
- Low-grade fever associated with seizure onset (<39 degrees Celsius)
- Short duration of fever before the seizure(<1 hour)
- Complex febrile seizure
- Attendance at a daycare nursery—presumed increased viral exposure
Case studies
Case 1
An 18-months old girl, fully immunised came with sudden onset loss of control and seizure activity. History of 4 days of fever but no respiratory or GI symptoms. She has a history of febrile seizures as a toddler.
Diagnosis
On examination, the child was fatigued, and alert, with no distress or signs of dehydration. Vitals within normal limits, temp 37.4, normal capillary refill and colour. Her respiratory, abdominal and ENT exams are unremarkable. neurological exam was normal.
Management
This is a case of recurrence of typical febrile convulsion, which as discussed occurs in 30% of pts with febrile convulsion. Management was symptomatic and proper counselling of parents.
Case 2
A 4-years old male child came with a history of fever and status epilepticus for the past hour before admission into PICU. Fever was moderate grade intermittent in nature. Convulsions were of GTCS type lasting for almost one hour involving both upper and lower limbs with up rolling of eyes and frothing from mouth. He had no faecal or urinary incontinence. There is a history of recurrent episodes of convulsions since 9 months of age.
Diagnosis
Skin examination showed as following;
- Multiple, soft dome-shaped lesions around the nose and cheek (adenoma sebaceum).
- Multiple hypo-pigmented, lanceolate macules with serrated edges on the back ( ash leaf macules).
His laboratory investigations revealed normal blood counts and routine urinalysis, X-ray chest was normal. Renal function test and serum electrolytes were normal. Ultrasonography of the kidneys showed a left-sided cortical renal cyst. Echocardiography of the heart revealed a mass of 1.6 x 1cm mass attached to the left ventricular apex suggestive of rhabdomyoma.
MRI brain showed multiple sub ependymal nodules/ hamartomas involving the bilateral lateral ventricles and in the left caudate nucleus s/o tuberous sclerosis
Management
Seizures were controlled with intravenous phenytoin which was changed over to oral maintenance and also started on sodium valproate and phenytoin was slowly tapered off and stopped and was discharged after 2 weeks and was advised for regular follow-up.
This was a unique case of tuberous sclerosis presenting as febrile convulsion which on thorough physical examination helped in unearthing the diagnosis and correct management.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Rajiv Balan is a practising neonatologist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries