Patient Monitoring and Follow-Up: Importance of Continuity of Care in Chronic Disease Management
M3 India Newsdesk Apr 21, 2024
Unveil the pivotal role of Continuity of Care (COC) in chronic disease management, from enhancing outcomes to fostering trust. Explore how this multifaceted approach is reshaping global healthcare delivery.
Globally there is an increased incidence of suffering, morbidity and mortality due to chronic diseases such as diabetes, hypertension, end-stage renal disease, cancer etc. This in turn has posed a public health burden and financial strain with health sector costs predicted to touch 7 trillion dollars by 2025.
Chronic diseases as the name suggests are a long-term problem and the focus here is to improve the quality of life (QOL) of these patients in the long run and to reduce long-term morbidity and mortality.
COC has gained momentum in recent times at the primary health care level. The evolution of the healthcare system into a complex model involving multiple service providers, technical and technological advancements such as the electronic medical record, and intranet usage for communication between departments are some of the potential causes for this increased recognition.
There is evidence to suggest that COC is causing a significant reduction in hospital admissions, ER admissions and healthcare costs. It also shows increased patient satisfaction and trust in their respective healthcare providers which leads to better delivery of people-centred health services. Continuity of Care has been defined as:
McGraw Hill definition: “Uninterrupted healthcare for a condition from the time of first contact to the point of resolution or long-term maintenance”.
WHO definition: COC is the degree to which people experience a series of discrete healthcare events as coherent and interconnected over time and consistent with their health needs and preferences.
Both COC and care coordination are interrelated. Continuity of Care permits care coordination by creating relationships to support seamless relations among numerous providers within interdisciplinary teams or across care settings or sectors. Three types of COC have been identified.
Informational Continuity (IC): Refers to the extent to which patient's medical records of previous visits, investigations, management etc are utilised to improve the current visit or care plan. Also emphasises clear, thorough, detailed transfer of information between different departments so that it is consistent, updated, and accessible for all healthcare providers.
Relational Continuity (RC): This signifies the therapeutic connection between the patient and all related providers, where current and old care management is well connected to the future management plan.
Management Continuity (MC): It encompasses timely care delivery more comprehensively and consistently parallels to a standard management plan. Emphasis is given to the content of care plans to ensure consistency. MC is characterised by:
Interpersonal Continuity (IPC): This is basically the trustable relation between the patients and health care providers, long-term consistent care and Adaptable health care to meet the patient's personal, behavioural, cultural, and family needs.
Longitudinal Continuity (LC): Essentially, it entails the chronicle of engagements and exchanges with a comparable healthcare professional across various instances. It holds significant ties to the following elements:
- Discharge from home and the subsequent plan for follow-up visits to healthcare provider locations, irrespective of the level of care.
- Transparent protocols for referrals to and from each tier of care.
- Guidance on care or facilitation within the community.
- Support from family and external social networks.
Importance of Continuity of Care (COC)
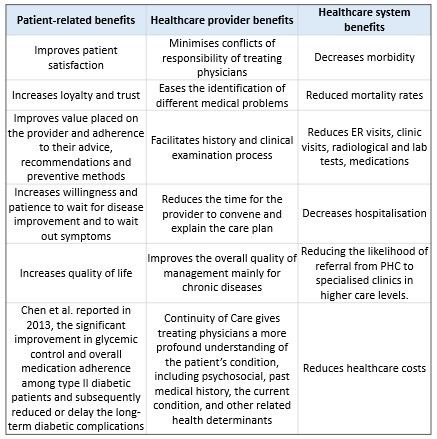
Several studies in family practice and primary care have established the benefits of COC as seen in the table below. Gray et al. reported a reduced all-cause mortality rate associated with COC, through a systematic review with a meta-analysis conducted in 2018.
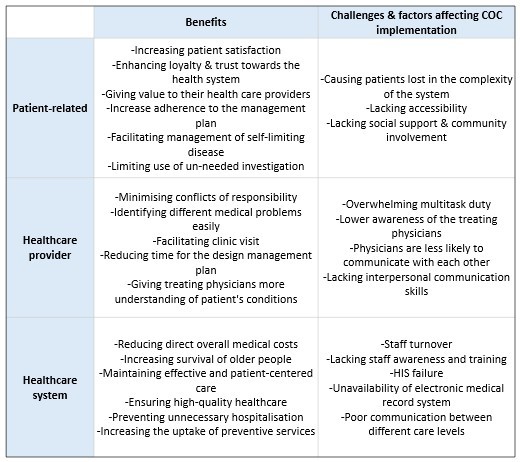
Challenges and factors affecting proper Continuity of Care implementation
Barriers and factors that influence the COC can be stratified into three main categories as follows:
Measurement of Continuity of Care measuring IC through transfer information
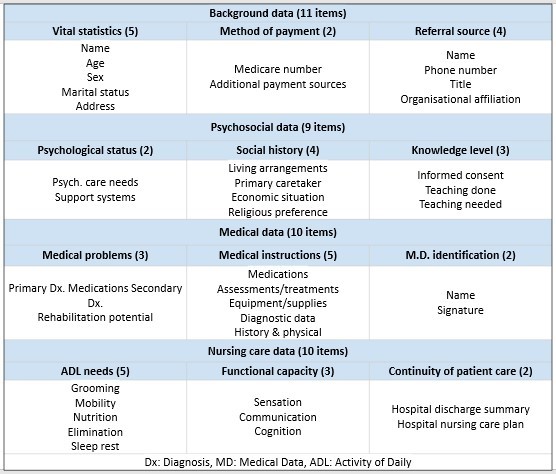
A widely acknowledged instrument is the Referral Data Inventory (RDI) established by Anderson & Helms in 1995. It evaluates four primary categories of patient data: background information, psychosocial details, medical history, and nursing considerations. Comprising a total of 40 items, completion of the RDI is crucial to ensure comprehensive information transfer among healthcare providers or across various levels of care, as outlined in the table.
IC through information usage
The Components of Primary Care Index (CPCI), Primary Care Assessment Survey (PCAS), and Primary Care Assessment Tool (PCAT) can be used.
Measurement of relational continuity
Assessment of affiliation between the patient and healthcare providers
Traditionally, surveys involve questioning patients regarding the identity of their regular healthcare providers or whether they consistently see the same healthcare provider during visits to the same clinic or specialist. This information can be retrieved from the Hospital Information System (HIS) or any other electronic medical record system.
Evaluation of the strength of the patient-provider relationship
Survey inquiries regarding the depth of the patient-healthcare provider connection can be conducted regularly or during each visit. Additionally, satisfaction surveys such as the Chao Perception of Continuity Scale, Alberta Continuity of Services Scale for Mental Health (ACSS-MH), Care Continuity Across Levels of Care Scale, and the Nijmegen Continuity Questionnaire (available in two versions) can also be utilised for this purpose.
Assessment of evidence of longitudinal follow-up
Examining the time lapse between the issuance of management prescriptions and subsequent follow-up appointments.
- Tracking missed appointments or the rate of no-shows. A higher occurrence of no-shows suggests insufficient management continuity in longitudinal follow-ups.
- Utilising the Temporal Continuity Index (TCI) to assess the intervals between the initial index visit and subsequent follow-up appointments relative to expected durations.
- Assessing treatment or management completion rates, This metric is particularly relevant for chronic conditions requiring long-term medication regimens, such as chronic hepatitis infections
- Evaluating adherence to disease-specific protocols and the consistency of care over time by auditing and assessing the extent to which various healthcare providers adhere to the primary management plan across different points in time.
Measurement of longitudinal or chronology of Continuity of Care
Assessing duration and intensity of patient/provider affiliation
This can be accomplished by extracting data from the patient's medical records or conducting a survey, which assesses the following:
The duration of time between the initial assessment visit and the last encounter between the patient and the healthcare provider, thereby quantifying the attrition rate of patients over a defined time period. High attrition rates signify a significant number of patients either missing follow-up appointments or discontinuing care.
Tools like PCAT and CCAENA can be used to assess different aspects of Continuity of Care (COC) are employed to determine the duration and intensity of patient/provider affiliation.
Concentration of care among different providers in sequential care
Can be evaluated by examining the number of distinct healthcare providers with whom a patient has interacted within a specified time frame or hospital admission.
- The Usual Provider of Care (UPC) index, which is calculated as the ratio of the total number of visits to the usual healthcare provider to the total number of visits over a specific period.
- The Continuity of Care (COC) index, which assesses both the concentration and dispersion of care. Less commonly used indices that also measure these aspects include FRAC, CON, and the K-index.
Sequential care measurements
The Sequential Continuity Index (SECON) stands as a widely acknowledged metric used for gauging the consistency of patients' visits with a particular healthcare provider or institution.
The Alpha Index CIα, portrays the average sequential continuity as well as the concentration of providers throughout a specified timeframe.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Akshayaa is a General Practitioner at Sri. Balaji Heart Centre, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries