Oxygen therapy strategies in COVID: New Indian guideline
M3 India Newsdesk May 03, 2021
The expert consensus guidelines for 2021 COVID-19 management with Indian context has been finely framed and checked. Because there are so many standards and not everyone agrees to the same treatment, physicians should use their own judgement, particularly when recommendations are constantly evolving. This guideline is aimed squarely at the current second wave and deals with oxygen therapy strategies in COVID.
For our comprehensive coverage and latest updates on COVID-19 click here.
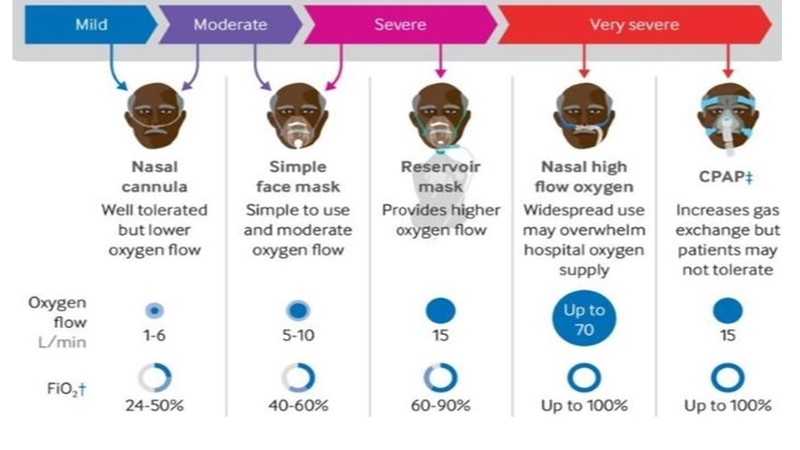
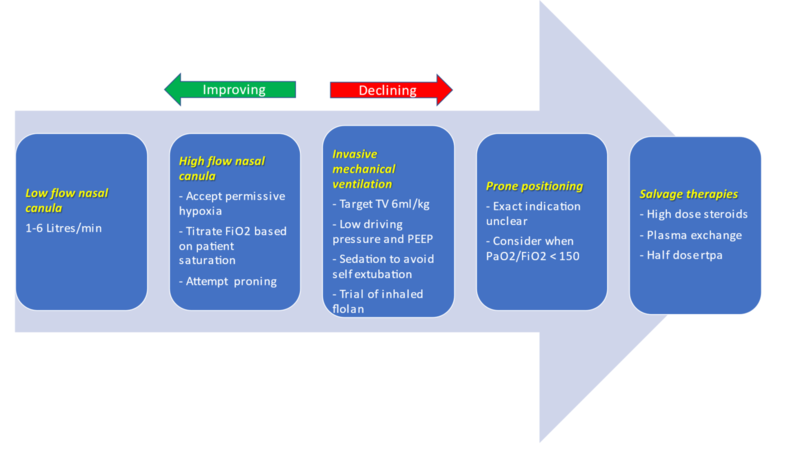
Oxygen therapy strategies in COVID
Source: Provided in Reference [12]
- Enhance oxygenation: Target saturation should be greater than 96% in those without type 2 respiratory failure and between 88 and 92% in those with hypercapnic respiratory failure.
- Reduce respiratory work: Respiratory rate should be <35 breaths per minute with no use of accessory muscles of respiration.
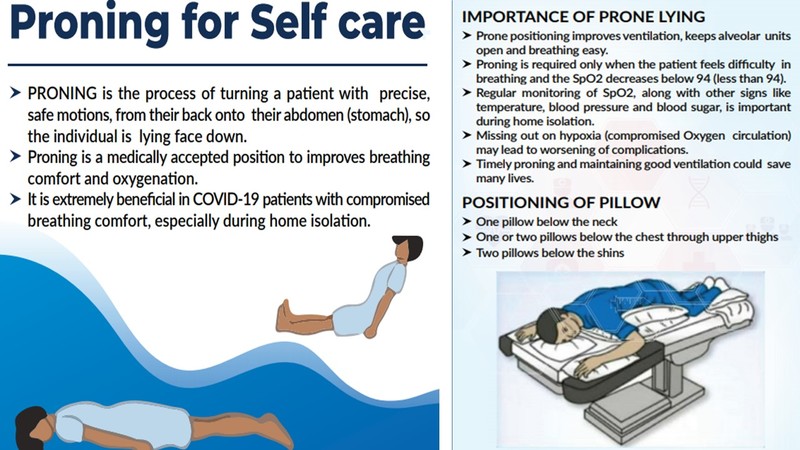
The technique for awake self-proning is as follows:
- Observation: Regular checks of O2 levels is expected. For continuous surveillance, ECG leads should be attached to the posterior chest wall.
- Prior to proning: Prepare for toileting, feeding, and oral medication administration prior to proning. If necessary, place the bed in reverse Trendelenburg (head above bottom, 10 degrees) to help relieve intraocular pressure.
- Assure that the patient's bladder is empty.
- Educate and inform the patient. Explain to the patient the process and reason for the intervention.
- To reduce the chance of dislodging, route tubing towards the top of the pad, not around the patient. Ascertain that all support instruments are securely attached to the patient. For example, place a sleeve over the IV access site and position the urinary catheter.
- Examine pressure points to prevent skin breakdown.
The protocol for prone placement is as follows:
- The patient should lie on their stomach with their arms at their sides or in the "swimmer" pose
- If a patient is unable to handle, they can rotate to lateral decubitus or partly prop to the side (between pronation and lateral decubitus), as desired, with pillows and with cushioning. Since there is actually no evidence on which side positioning is beneficial, the patient should be entirely prone instead of on the side.
- Check to ensure that oxygen saturation has not declined 15 minutes after each location transition. If it has, attempt a different position.
- If the patient's oxygen saturation level drops significantly, the following steps should be taken:
- Verify that the patient's oxygen supply is connected to the wall and is correctly positioned on the patient (this is a common cause of desaturation).
- Request that the patient is changed to a different position as described previously.
- If the patient's saturations have not risen to pre-treatment thresholds after 10 minutes, recommend escalating oxygen therapy via the same/different mode.
Source: Provided in Reference [13]

Source: Provided in Reference [13]
Amount of time spent proning
Proning should be attempted every 4 hours, and the patient should remain prone for as long as possible. The patient's anxiety frequently prevents them from proning, but they should be allowed to set realistic deadlines, such as 1 to 2 hours (or more if possible). The optimal time frame is 16 hours every 24 hours (e.g. 4 times for 4 hours each session).
When do you avoid proning while awake?
- A patient has the option of ceasing to pronate when conscious at any moment
- In the event of haemodynamic dysfunction or imminent respiratory collapse, the clinician should avoid proning and consider intubation
Awake self-proning contraindications
Haemodynamic dysfunction (on vasoactive medications): vulnerable. These patients in a controlled setting are preferable, if they are suffering from severe/refractory haemodynamic instability,
Proning is not recommended if:
- Intracranial pressure has risen
- Abdominal pressure has increased
- Wounds to the abdomen, chest, and face
- Precautions for the cervical spine
- Obesity to the extreme
- GCS less than eight
- Second to third trimester of pregnancy
Selection of patients for non-invasive ventilation (NIV) use
Step 1- A cause of respiratory failure that is likely to improve with NIV
Step 2- Using clinical and blood gas criteria, identify patients that need ventilatory assistance; dyspnoea, tachypnoea, and imminent respiratory muscle weakness range from mild to extreme
Step 3- Avoid patients who may be at risk from NIV
Prognostic factors for NIV effectiveness in patients with acute respiratory failure
- Reduced disease acuity (APACHE score)
- Cooperation ability; higher neurologic score (GCS <10)
- Capacity to regulate one's breathing in conjunction with a ventilator
- Hypercarbia, but not excessively so (PaCO2 difference between 45 and 92 mmHg)
- Acidemia, but not to an abnormal degree (pH between 7.1 and 7.35)
Contraindications for the use of NIV
- Cardiac/respiratory arrest or emergency intubation needed
- Encephalopathy with severe severity (e.g. GCS 10)
- Severe gastrointestinal bleeding
- Instability of the haemodynamic system or an unstable heart arrhythmia
- Surgery on the face or the nervous system, trauma, or deformity
- Obstruction of the upper airway
- Lack of cooperation/protection of the airway
- Incapacity to expel secretions/risk of aspiration
- Pneumothorax left untreated
Therapies under investigation
- Convalescent plasma: CP treatment can be considered in high-risk patients (>75 years of age or >65 years of age with co-morbidities) who present within three days of symptom initiation. Plasma should be obtained from recovered COVID-19 subjects with elevated antibody titres. The dosage is 200–250 ml, followed by a second dose 24 hours later if required. Convalescent plasma was not associated with a decrease in the progression of extreme COVID-19 or all-cause mortality in a prominent open-label phase II multicenter randomised randomized experiment (PLACID Trial).
- Colchicine: It should be considered within 24 hours of a positive result in high-risk patients >65 years. The dosage is 0.5 mg BD for three days followed by 0.5 mg OD before the acute disease resolves. However, recently updated NIH guidelines did not find evidence in favour or against colchicine.
- Baricitinib: It can be administered in addition with remdesivir in patients with extreme COVID 19 who cannot be treated with steroids, 4 mg once daily for 14 days. It is a promising medication, especially in patients with co-morbidities. Hyperglycaemia is a serious issue. Along with remdesivir, it is widely used as a steroid-sparing agent in place of corticosteroids. The fact that it is a once-a-day oral treatment contributes to its compliance.
- Baricitinib plus remdesivir for COVID-infected patients hospitalised: Baricitinib plus remdesivir is preferable to remdesivir alone in lowering recovery time and improving clinical progress in patients with COVID-19, including those with severe disease receiving supplemental oxygen or non-invasive ventilation at a high flow rate. The mixture has been linked to a decreased risk of severe adverse effects. Olumiant4 (Eli Lilly) is obtainable in India through online pharmacies. Tofacitinib 5 mg is another JAK inhibitor that is readily available.
- Monoclonal antibodies are being used in COVID-19 cases in the United States: Bamlanivimab infusion or casirivimab and imdevimab combined cuts hospitalisation by 70% in moderately ill COVID-19 patients.
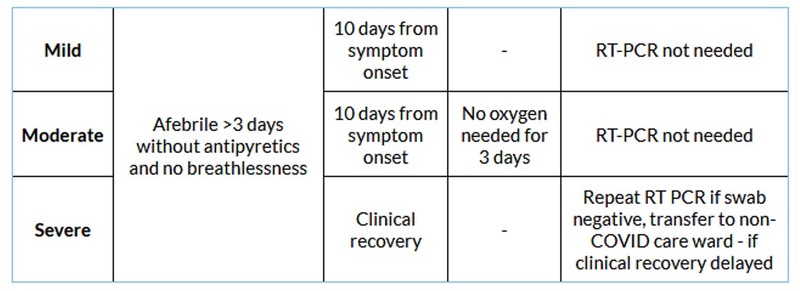
- Discharge Strategy: Comply to any state-specific rules that might exist.
Discharge criteria
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Monish S Raut is a Consultant in Cardiothoracic Vascular Anaesthesiology. His area of expertise is perioperative management and echocardiography with numerous publications in various national and international indexed journals.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries