NICE 2021 update: Headache assessment & treatment summary
M3 India Newsdesk Sep 08, 2021
Headache is a very common condition that can be managed and treated provided they are assessed and the type diagnosed correctly. This guideline article provides top summary points from updated recommendations by NICE about the different types of headaches and suitable treatment interventions.
The National Institute for Health and Care Excellence has published an updated guideline on the diagnosis and management of tension-type headache, migraine (including migraine with aura and menstrual-related migraine), cluster headache, and medication overuse headache in adolescents and adults (aged 12 years and older).
It seeks to enhance headache detection and management through more targeted therapy, so improving the quality of life of those who suffer from headaches and avoiding needless examinations. The following recommendations have been recognised as 2012 implementation priorities. In 2015, the evidence for the critical priority advice on preventive therapy was reviewed, but the recommended action remained unchanged.
Note: MHRA suggestion on antiepileptic drugs during pregnancy
In May 2021, NICE updated its recommendation for topiramate for migraine prophylaxis to include discussion of potential benefits and risks, as well as the critical importance of effective contraception for women and girls of childbearing potential who are taking topiramate.
Assessment, diagnosis, and management were used to categorise the recommendations. They have been condensed and summarised here.
Assessment
Evaluate individuals who appear with headache and any of the following characteristics, and decide if additional investigations and/or referral is necessary:
- Headache that worsens with fever, sudden onset headache that reaches maximum intensity within 5 minutes, new-onset neurological deficit, new-onset cognitive dysfunction, personality change, impaired level of consciousness, recent (typically within the last 3 months) head trauma, headache triggered by coughing, Valsalva (attempting to breathe out with nose and mouth blocked), sneezing, or headache triggered by exercise.
- Consider additional tests and/or referral for individuals who report a new-onset headache and one or more of the following:
- Impaired immunity, for example, as a result of HIV or immunosuppressive drugs
- Age less than 20 years and a history of malignancy
- A history of malignancy known to metastasise to the brain
- Vomiting for no apparent reason
- Consider keeping a headache record to assist with primary headache diagnosis.
- If a headache diary is employed, request that the individual keep track of the following for a minimum of 8 weeks. The patient can record the following for a minimum of 8 weeks:
- Frequency
- Duration and intensity of headaches
- Any related symptoms
- All prescribed and over-the-counter drugs used to treat headaches
- Possible precipitants
- The relationship of headaches to menstruation
Diagnosis
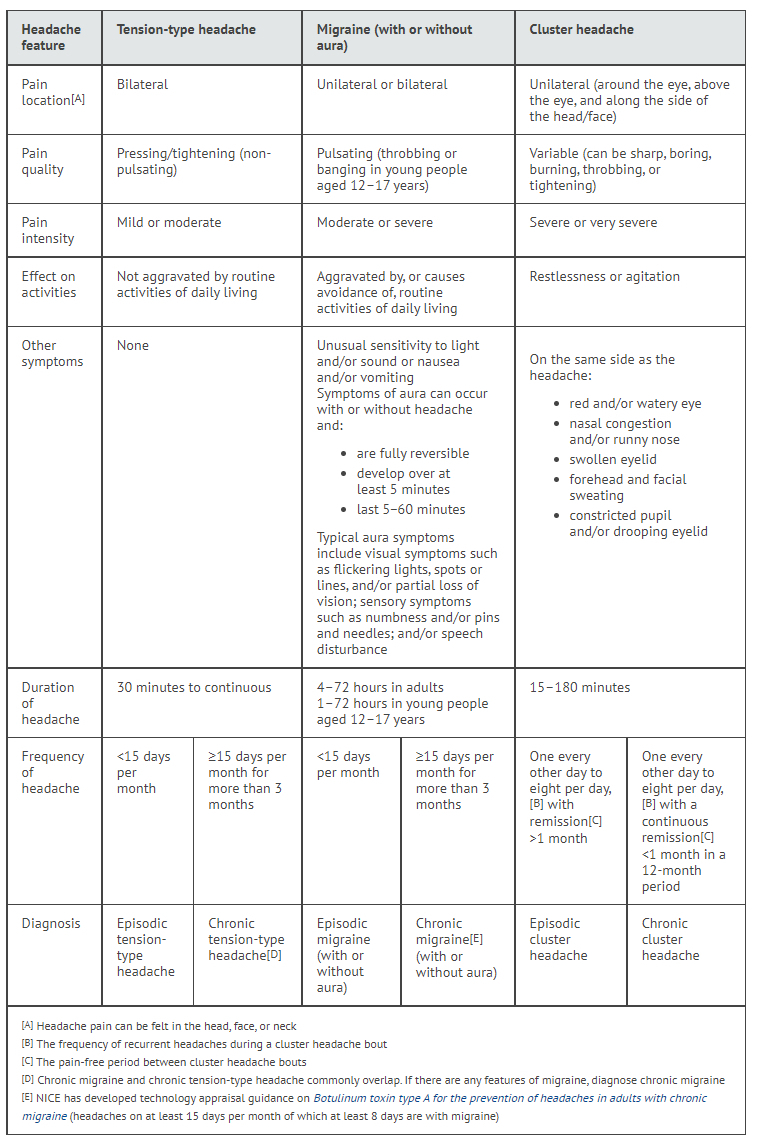
Tension headaches, migraines (with or without aura), and cluster headaches are all types of headaches. Diagnose tension headaches, migraines, or cluster headaches using the headache characteristics listed in Table 1. Persistent migraines and chronic tension headaches frequently occur together. Chronic migraine can be diagnosed if any of the symptoms of migraine are present.
- Tension headaches are of the episodic kind and occur on less than 15 days per month.
- Chronic tension headaches occur every 15 or more days per month over a period of at least three months.
- Episodic cluster headaches occur on an irregular basis, ranging from once every other day to eight times a day, with a pain-free interval of more than one month in between.
- Chronic cluster headaches occur on average every other day to eight times a day, with a pain-free period of less than one month in a 12-month period.
Table 1: Headache features according to headache type [1]
Migraine with aura
Suspect aura in individuals who appear with or without a headache and neurological symptoms that are completely reversible and develop gradually, either alone or in succession, over a minimum of 5 minutes and persist for 5 to 60 minutes.
Diagnose migraine with aura in individuals who appear with or without a headache and exhibit one or more of the following typical aura symptoms that match the recommended criteria:
- Positive and/or negative visual symptoms like flashing lights, dots or lines (for example, partial loss of vision) sensory sensations that may be pleasant (pins and needles, for example)
- Negative (numbness, for example) speaking impediment
For persons who appear with or without a migraine headache and any of the following atypical aura symptoms that match the criteria in the guideline, consider additional examinations and/or referral. The following are all examples of visual symptoms:
- Motor weakness
- Double vision
- Visual symptoms affecting only one eye
- Impaired balance, or a lowered degree of consciousness
Menstrual‑related migraine
Suspect menstrual migraine in women and girls who have migraines mostly 2 days before and 3 days after the start of menstruation in at least 2 of 3 consecutive menstrual cycles. It is advisable to keep a headache journal for at least two menstrual cycles to diagnose menstrual migraines.
Medication overuse headache
Be aware of the possibility of medication overuse headache in people who developed or worsened their headache while taking the following drugs for 3 months or more- Triptans, opioids, ergots, or combination analgesic medications for 10 days or more per month, or paracetamol, aspirin, or an NSAID for 15 days or more per month, either alone or in any combination.
Treatment recommendations for different types of headaches
Tension‑type headache
Acute treatment:
- For immediate treatment of tension-type headaches, consider aspirin, paracetamol, or an NSAID, taking into account the person's preference, comorbidities, and risk of adverse effects. Aspirin-containing preparations should not be given to children under the age of 16 due to the risk of Reye's syndrome.
- Do not prescribe opioids for the treatment of tension headaches.
Prophylactic therapy: Think about a course of up to 10 acupuncture treatments spread out over 5 to 8 weeks for the preventative treatment of persistent tension-type headache.
Migraine with or without aura
Acute treatment:
- For the immediate treatment of migraine, offer combination therapy with an oral triptan and an NSAID, or an oral triptan and paracetamol, taking into consideration the person's preference, comorbidities, and risk of side effects. Consider a nasal triptan instead of an oral triptan for young people aged 12 to 17 years. This was an off-label usage of triptans (excluding nasal sumatriptan) in children under the age of 18 in November 2015.
- Consider monotherapy with an oral triptan, NSAID, aspirin (900 mg), or paracetamol for the immediate treatment of migraine, taking into account the person's choice, comorbidities, and risk of adverse effects. This was an off-label usage of triptans in children under the age of 18 in November 2015.
- When prescribing a triptan, begin with the lowest acquisition cost. If this is frequently unsuccessful, consider one or more different triptans. In November 2015, this was an off-label usage of triptans in children under the age of 18. Consider an antiemetic in addition to other acute migraine treatments, even if nausea and vomiting are not present.
- Do not provide ergots or opioids for acute migraine therapy. If oral preparations (or nasal preparations in young persons aged 12 to 17 years) are unsuccessful or poorly tolerated for the immediate treatment of migraine, administer a non-oral preparation of metoclopramide or prochlorperazine and consider adding a nonoral NSAID or triptan if these have not been tried.
- Only a buccal formulation of prochlorperazine was approved for this use in November 2015 (prochlorperazine was approved for nausea and vomiting treatment). Nasal sumatriptan was the only triptan licenced for this use in children under the age of 18. This was an off-label use of metoclopramide in children and adolescents.
Prophylactic treatment:
- Discuss with the individual the advantages and dangers of migraine preventative medication, taking into consideration the person's preference, comorbidities, risk of adverse events, and the impact of the headache on their quality of life.
- After a thorough discussion of the advantages and dangers of each choice, recommend topiramate or propranolol for migraine prevention. Include in the discussion:
- The potential benefit of topiramate in reducing migraine recurrence and severity
- The risk of foetal malformations with topiramate
- The risk of decreased effectiveness of hormonal contraceptives with topiramate
- The importance of effective contraception for women and girls of childbearing potential who are taking topiramate (for example, by using medroxyprogesterone acetate depot injection)
People who suffer from depression or migraines may be more likely to use propranolol for self-harm. According to the Healthcare Safety Investigation Branch's assessment on the under-recognised risk of injury from propranolol, use caution while giving it.
- Consider amitriptyline for migraine prophylaxis based on the individual's desire, comorbidities, and risk of adverse effects.
- Do not prescribe gabapentin as a migraine preventative.
- If both topiramate and propranolol are inappropriate or unsuccessful, try a course of up to 10 sessions of acupuncture spread over 5 to 8 weeks, depending on the person's choice, comorbidities, and risk of adverse effects.
- Continue existing medication as needed for persons who are already receiving another kind of prophylaxis and whose migraine is well managed.
- Reconsider the necessity for ongoing migraine prophylaxis 6 months after starting preventative therapy.
- Inform migraine sufferers that riboflavin (400 mg once daily) may be useful in lowering migraine frequency and intensity in some persons.
- Do not routinely provide combination hormonal contraception to women and girls who have migraines with aura for contraception.
Menstrual-related migraine
- Consider therapy with frovatriptan (2.5 mg twice a day) or zolmitriptan (2.5 mg twice or three times a day) on the days migraine is predicted for women and girls who do not react sufficiently to normal acute therapy.
- Give pregnant women paracetamol for acute migraine therapy.
- After considering the woman's need for therapy and the dangers associated with each drug during pregnancy, consider using a triptan or an NSAID.
- If preventative migraine therapy is required during pregnancy, seek the counsel of a professional.
Cluster headache
Acute treatment:
- Consult a GP with a specific interest in headaches or a neurologist about the necessity for neuroimaging for persons experiencing their first attack of cluster headaches.
- For the immediate treatment of cluster headache, provide oxygen and/or a subcutaneous or nasal triptan.
- When utilising oxygen for the acute treatment of cluster headache, utilise 100% oxygen at a flow rate of at least 12 litres per minute with a nonrebreathing mask and a reservoir bag, and arrange for home and ambulatory oxygen supplies.
- When utilising a subcutaneous or nasal triptan, ensure that the individual is given an appropriate supply of triptans based on their history of cluster episodes and the manufacturer's maximum daily dose. This was an off-label usage of subcutaneous triptans in children under the age of 18 in November 2015.
- Do not provide paracetamol, NSAIDs, opioids, ergots, or oral triptans for the management of cluster headaches.
Prophylactic treatment:
- Consider using verapamil as a preventative measure during a cluster headache attack. If you are inexperienced with the use of verapamil for cluster headache, obtain medical counsel before beginning it, particularly guidance on ECG monitoring.
- Seek medical attention if your cluster headache does not respond to verapamil. This was an off-label usage of verapamil in November 2015. NICE's prescription information may be found here.
- If therapy for cluster headaches is required during pregnancy, seek the counsel of a professional.
Medication overuse headache
- Explain to patients suffering from medication overuse headache that it will be addressed by discontinuing the overused medicine.
- Advise individuals to discontinue all over-the-counter severe headache treatments for at least one month, and to discontinue suddenly rather than gradually.
- Inform them that their headache symptoms are likely to worsen in the near term before improving and that there may be associated withdrawal symptoms, and offer them attentive follow-up and assistance as needed.
- For persons with medication overuse headache, consider preventive therapy for the underlying main headache condition in addition to discontinuation of the overused drug.
- Do not give inpatient withdrawal for medication overuse headaches on a regular basis.
- Consider expert referral and/or inpatient withdrawal of overused medicine for patients who take powerful opioids, have related comorbidities, or have previously failed efforts at the withdrawal of overused medicine.
- Re-examine the diagnosis of medication overuse headache and its subsequent care.
- Review and manage 4 to 8 weeks following the start of medication discontinuation.
Management
All headache disorders
- Think about keeping a headache journal to track the frequency, length, and intensity of headaches, to track the success of headache therapies, and to use as a starting point for a conversation with the individual about their headache problem and its effects.
- If a person is diagnosed with a headache problem develops any of the characteristics specified in the recommendations, consider additional examinations and/or referral.
- Do not refer persons with tension headaches, migraines, cluster headaches, or medication overuse headaches to neuroimaging for the sole purpose of reassurance.
Information and support for people with headache disorders
Include the following in discussions with the person suffering from a headache disorder:
- A positive diagnosis, including an explanation of the diagnosis and reassurance that other pathology has been ruled out, management options, and recognition that headache is a valid medical disorder that can have a significant impact on the person and their family or caregivers.
- Provide the person with written and spoken information regarding headache problems, as well as contact information for support groups.
- Educate persons who are receiving acute therapy for their headache issue about the dangers of drug overuse.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries