New 2nd wave guidance for COVID-19 management in pregnancy
M3 India Newsdesk May 15, 2021
According to the largest systematic study, pregnant women are not at greater risk of dying from COVID-19. Pregnant women with symptomatic COVID-19 who need hospitalisation have overall poorer maternal outcomes, including an elevated risk of death, but this risk remains extremely low (the UK maternal mortality rate from COVID-19 is 2.2 per 100,000 maternities). This guideline is a 2021 consensus aimed specifically at the current second wave. The article deals with the management of pregnancy in COVID after compiling various recommendations from major societies.
For our comprehensive coverage and latest updates on COVID-19 click here.
The guideline structure
While the guideline has been finely framed and checked because there are so many standards and not everyone agrees to the same treatment, physicians should use their own judgement, particularly when recommendations are constantly evolving. Pregnant women with COVID-19 have a higher risk of intensive care unit (ICU) admittance than non-pregnant women with COVID-19. This may represent a lower limit for ICU admission, rather than more acute illness.
Factors associated with hospitalisation for COVID-19 infection during pregnancy
The following risk factors tend to be linked with both infection and hospitalisation with COVID-19:
- African, Asian, and minority ethnic (BAME) ancestry
- Possessing a BMI of 25 kg/m2 or greater
- Co-morbidity prior to birth, such as pre-existing diabetes or chronic hypertension
- Maternal age of at least 35 years
- Residing in areas or households with elevated socioeconomic poverty (non-pregnancy data)
COVID-19's impact on the foetus
Significant findings include:
- COVID-19 infection in pregnant women is associated with an elevated risk of iatrogenic preterm delivery.
- With the exception of preterm delivery, there is no proof that COVID-19 infection has a detrimental impact on the foetus or neonatal outcomes.
Important factors to remember while caring for symptomatic women with suspected or verified COVID-19
Preparation for birth
- If a home-birth or birth in a midwife-led unit is expected, a conversation with the mother about the possibility for foetal compromise during the active period of pregnancy should be undertaken if she is symptomatic for SARS-CoV-2.
- Attending an obstetric unit where the baby can be monitored continuously via electronic foetal monitoring (CEFM) should be recommended for delivery.
The delivery process
- Birth timing: A good COVID-19 outcome in an otherwise healthy woman with no signs of foetal compromise is not a reason to rush birth.
- Induction of labour (IOL): It is associated with a longer length of stay in the hospital than spontaneous labour. Examine the indication for IOL and determine if the anticipated benefits exceed the potential risks. Wherever practicable, evaluate the availability and feasibility of outpatient IOLs.
- Mode of birth: Since there is presently no data to suggest that one mode of birth is preferable to another in women who are SARS-CoV-2 positive, the mode of birth should be openly discussed with the mother, taking her desires and any obstetric indications for intervention into account. The involvement of COVID-19 does not affect the mode of birth only if the woman's respiratory condition necessitates immediate action for birth.
- Respect and approval: Women must retain the ability to make wise choices about the treatment they receive.
- Monitoring the foetus: Discuss with women the various options for foetal monitoring during labour in compliance with current NICE recommendations. CEFM is recommended for women who exhibit symptoms of COVID-19. Current diagnosis with SARS-CoV-2 does not preclude the application of a foetal scalp electrode or the collection of foetal blood.
Analgesia
There is no proof that epidural, spinal, or anaesthetic analgesia or anaesthesia was contraindicated in the presence of coronaviruses. Epidural analgesia should also be suggested to women who are suspected or proven to have COVID-19 during labour to avoid the need for general anaesthesia.
Intrapartum care
- When a woman is transferred to the maternity suite with reported or suspected COVID-19, the appropriate members of the multidisciplinary team should be notified: Obstetrician specialist, anaesthetist consultant, midwife-in-charge, neonatologist consultant, neonatal nurse-in-charge, and infection management unit.
- Maternal assessments and evaluations can be continued as normal, with the inclusion of hourly oxygen saturations.
- Maintain an oxygen saturation of at least 94 per cent by adjusting oxygen therapy as required. If the woman has a fever, investigate and treat her according to the RCOG's sepsis guidelines for pregnant women.
Postpartum care
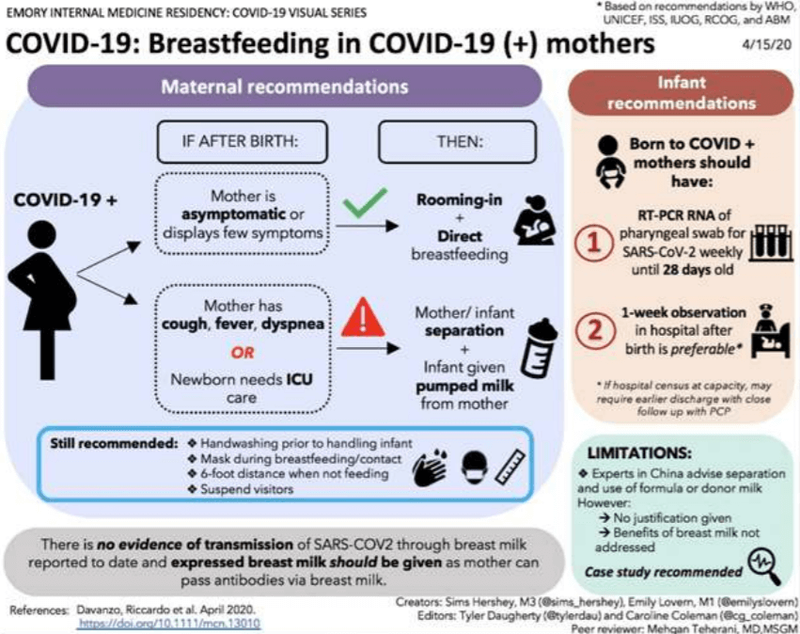
It is unclear if COVID-19-positive newborns are at an elevated risk of serious complications. Transmission after birth is a problem due to interaction with contagious respiratory secretions. Services should consider briefly removing the mother who has been diagnosed with COVID-19 or is a PUI from her baby (e.g., different rooms) before the mother's transmission-based measures are withdrawn.
Considerations for temporary separation
- The healthcare staff should explore the dangers and benefits of temporarily separating the mother from her baby.
- During their time as a PUI, the infant should be held in a separate isolation space.
- The decision to end the temporary isolation of the mother from her infant should be taken on an individual basis in coordination with physicians, infection prevention and management experts, and public health authorities.
- The nature of the disorder, the signs and symptoms of infection, and the effects of laboratory tests for the virus that causes COVID-19, SARS-CoV-2 in the mother and neonate should all be considered.
- If the newborn is colocated (also known as "rooming in") with his or her sick mother in the same hospital space as the mother's wishes or is necessary due to facility restrictions, hospitals should recommend introducing steps to decrease the vulnerability of the newborn to the COVID-19 virus.
- Consider employing engineering restraints such as physical obstacles (for example, a curtain between the mother and the newborn) and holding the newborn at least 6 feet away from the sick mother.
- A mother who has reported COVID-19 or is a PUI should put on a facemask and exercise hand hygiene before any feeding or any near contact with her newborn if no other responsible adult is present in the room to care for the newborn. The facemask should remain in place during contact with the newborn.
Practices to be continued when the mother is receiving transmission-based precautions in a medical facility
Breastfeeding: Mothers who wish to breastfeed should be allowed to express their breast milk through temporary separation to build and sustain milk supply. A designated breast pump should be given if necessary. Mothers should observe proper hand hygiene prior to expressing breast milk. Following each pumping session, thoroughly clean any pieces that come into contact with breast milk and disinfect the whole pump according to the manufacturer's instructions. A good caregiver should feed the newborn this expressed breast milk. If a mother and newborn stay in the same room and the mother wants to breastfeed, she should wear a facemask and exercise good hand hygiene before each feeding.
Discharge from the hospital: Postpartum women should be discharged according to the protocols for discharge of COVID-19-infected hospitalised patients. Maternal and foetal/neonatal conditions should be healthy.
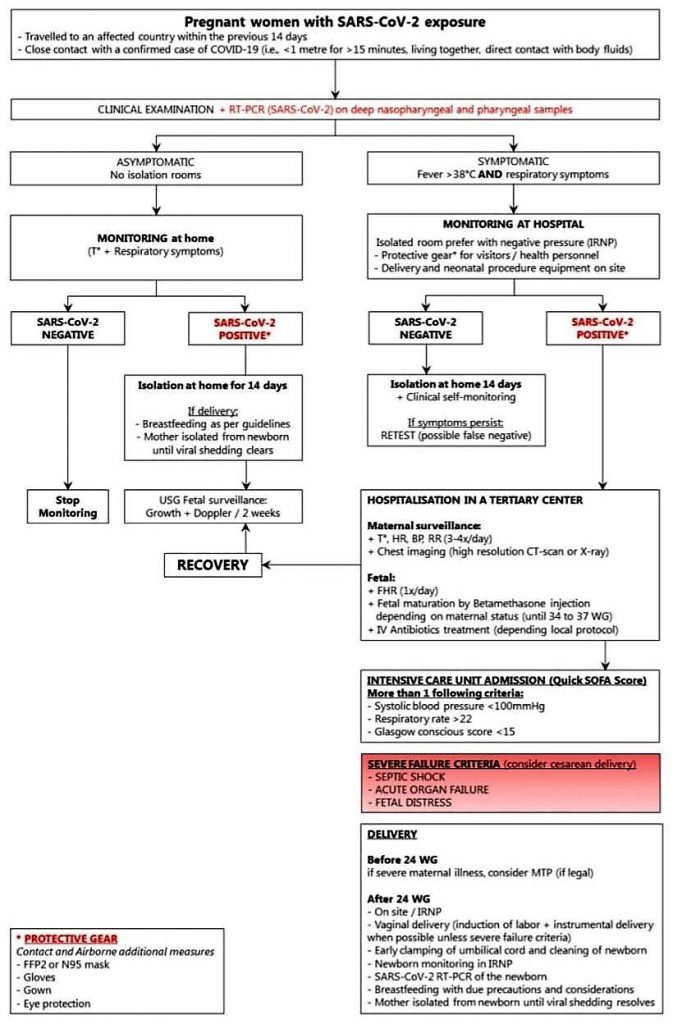
Pregnant Women's Management Flowchart (Adapted from The Lancet)
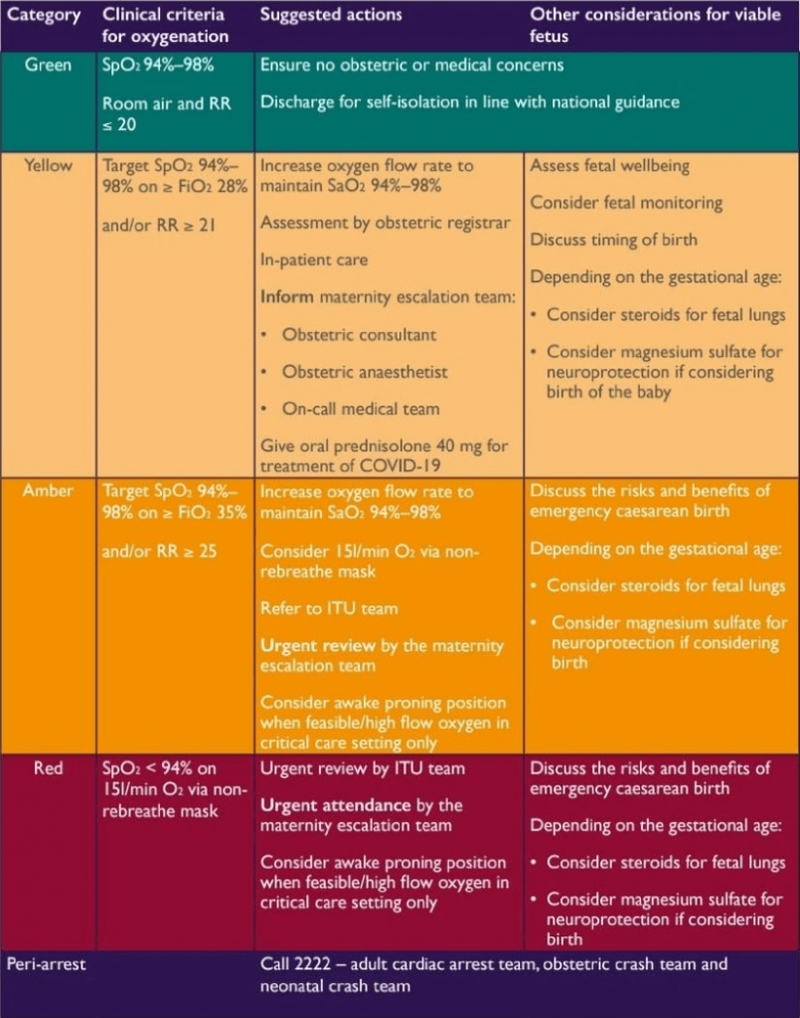
For women with alleged or reported COVID-19, an example of a pregnancy escalation strategy
(Adapted from Buy’s and St Thomas’ NHS Foundation Trust)
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries