Meningitis: A Comprehensive Approach to Diagnosis and Treatment
M3 India Newsdesk Mar 13, 2024
This article highlights the epidemiology, clinical features, diagnostic approach, and management protocols of the common causes of meningitis in the community.
Meningitis refers to an inflammatory condition affecting the meninges, the covering layers of the brain and spinal cord.
The three layers of meninges are
- The dura mater (pachymeninges)
- The arachnoid
- Pia matter (leptomeninges)
Besides infectious causes (bacteria, viral, fungal, etc.), meningitis can also occur due to some non-infectious aetiology.
Acute bacterial meningitis
Acute bacterial meningitis is a medical emergency, since delayed initiation of treatment results in an overall poor prognosis. Its common presenting features are fever, headache, and neck stiffness followed by clouding of the sensorium (meningoencephalitis)1. Typically, the symptoms progress over 3-4 days.
Causes
- The most common bacterial cause of meningitis in adults and children is S. pneumoniae 2. Splenectomy and low immunoglobulin levels are common predisposing factors.
- N. meningitidis, the second most common cause in adults, is associated with a purpuric rash.
- H. influenzae was previously most prevalent in children, but the incidence has reduced after increased vaccination. Staphylococcus species gain access to CNS through the breach of skin associated with trauma or surgery.
- L. monocytogenes causes meningitis in adults older than 65 years of age, immunocompromised and chronic alcohol abusers. These patients have associated ataxia and cranial nerve palsies.
Diagnosis
- CT scan is to be done before lumbar puncture if the patient has focal neurological deficits, clouded sensorium, new onset seizures or is immunocompromised 3.
- MRI may reveal T2 hyperintensity in the cerebral sulci and contrast enhancement of the leptomeninges. CSF studies reveal a polymorphonuclear (neutrophil predominant) lymphocytosis, elevated protein, and low glucose levels (Table 1).
- Microbiological diagnosis relies on gram stain and CSF culture, although PCR-based assays (e.g. BioFire FilmArray Meningitis/Encephalitis (ME) Panel)4 are nowadays being frequently used to hasten the diagnostic process.
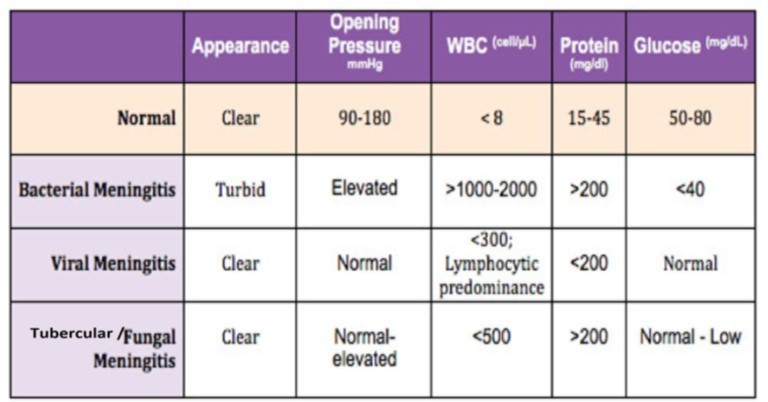
Table 1: CSF findings in Meningitis of various aetiology.
Treatment
Empirical Treatment of meningitis needs to be immediately initiated on suspicion of bacterial meningitis (Table 2). Although it is a routine practice to give Dexamethasone before or with the first dose of antibiotic, it has not been proven to be universally beneficial except in cases of streptococcal meningitis 5.
When culture reports are available, antibiotic dose and duration may be tailored to the specific organism.
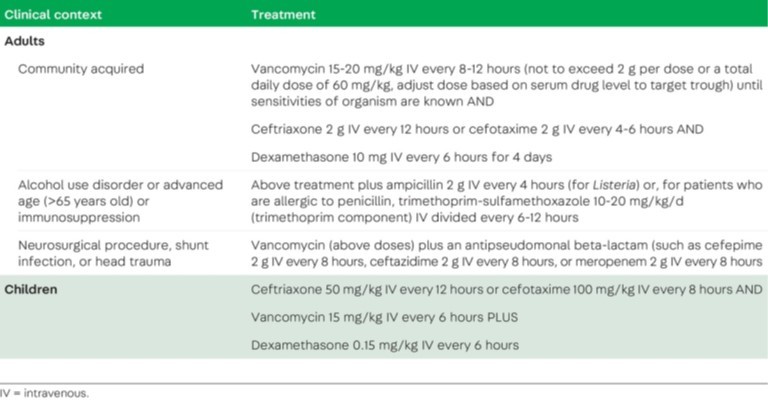
Table 2: Empirical treatment of Bacterial Meningitis
Acute viral meningitis
The symptoms of viral meningitis are less severe although similar to bacterial meningitis.
Causes
The most common causes of viral meningitis are enteroviruses (echoviruses, coxsackieviruses, and polioviruses), HSV-2, and VZV.
- Herpes Simplex Virus (HSV-2) meningitis can occur with or without genital infection, and at times can be recurrent (Mollaret Meningitis).
- Varicella Zoster Virus (VZV) can cause meningitis with or without the accompanying rash. It can also result in stroke secondary to vasculitis.
- Other agents responsible for causing viral meningitis include West Nile Virus and related arboviruses, Mumps virus, HIV and Lymphocytic Choriomeningitis Virus.
Diagnosis
- Neuroimaging is normal in most cases of viral meningitis.
- CSF studies reveal a lymphocytic pleocytosis with mostly normal glucose levels and mildly elevated protein levels.
- PCR is used to determine the aetiology in most cases, but some (e.g. arboviruses) are more readily diagnosed by serology.
Treatment
- Intravenous Acyclovir (10 mg/kg IV 3 times a day) is used to treat HSV-2 and VZV meningitis for 10-14 days.
- IV Immunoglobulin use has not shown any significant benefit in treating viral meningitis6.
Parasitic meningitis
- The free-living amoebae Naegleria fowleri and Angiostrongylus cantonensis tend to cause meningitis associated with Primary Amoebic Encephalitis.
- Meningitis can also occur with Granulomatous Amoebic Encephalitis caused by Balamuthia mandrillaris and Acanthamoeba.
- Naegleria infection enters through the nasopharynx and cribriform plate during swimming and is very much fatal.
- Angiostrongylus infection occurs via ingestion of contaminated seafood.
- CSF studies reveal eosinophilia and the organism can be detected on CSF wet-mount.
Various agents like Amphotericin B, miconazole, pentamidine, sulfadiazine, fluconazole and clarithromycin have been used with variable results.
Tubercular meningitis
Causes
- Mycobacterium tuberculosis is an important cause of meningitis in low and low-middle-income countries. The prevalence is also high amongst those who are immunocompromised.
- Clinical features like fever, headache, and neck stiffness usually present after a prodrome of 6 days 7. Besides these, tubercular meningitis can also present with some unusual features.
- Multiple cranial nerve palsies can occur secondary to basal meningeal involvement.
- Vasculitis can result in subcortical stroke, seizures (focal more common than generalised) are seen, hydrocephalus may develop, vision loss may be seen secondary to optochiasmatic arachnoiditis and transverse myelitis may also be seen.
- Besides, hyponatremia is a common complication associated with tubercular meningitis8.
Diagnosis
- CSF studies reveal lymphocytic pleocytosis, elevated protein and mildly reduced glucose. Neuroimaging (MRI preferable to CT) may reveal the lesions affecting the brainstem, basal ganglia, and midbrain (Fig 1).
- Initially, the Xpert MTB/RIF and now the Xpert MTB/RIF Ultra are recommended for diagnosis of tubercular meningitis as it has shown more sensitivity 9.
Treatment
- Treatment involves the use of anti-tubercular drugs isoniazid, rifampin, pyrazinamide, and ethambutol with the addition of dexamethasone in the initial phase of therapy.
- The intensive phase (HRZE/S) is given for a duration of 2 months followed by the continuation phase (HRE) for 8-10 months.
- In some instances (especially in HIV patients), a paradoxical worsening may occur after initiation of anti-tubercular therapy, known as IRIS.
- It is usually self-limited and may be managed with anti-inflammatory agents in mild cases and corticosteroids in severe cases, along with continuation of anti-tubercular therapy.
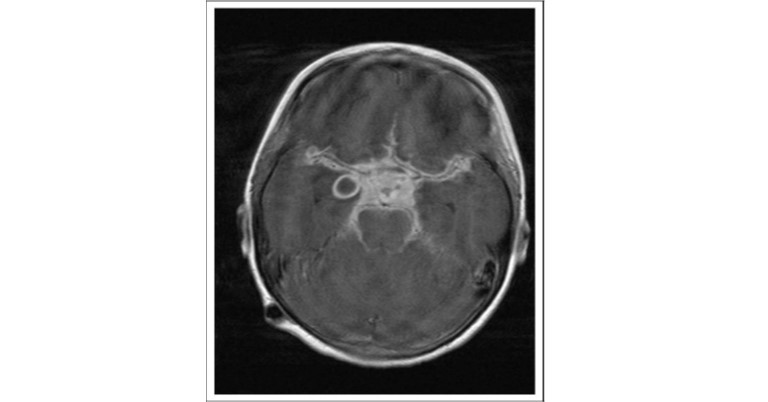
Fig 1: T1-weighted post gadolinium magnetic resonance imaging (MRI) scan demonstrates enhancement of the whole suprasellar cistern with displacement and compression of the optic nerve anteriorly. A ring-enhancing abscess associated with the right temporal lobe is also visible.
Fungal meningitis
Causes
- Fungi cause subacute to chronic meningitis and their incidence depends on the immune status of the patient, geography, and exposure history.
- Cryptococcal meningitis is the most common, mostly caused by C. neoformans. Most of the cases are seen in immunocompromised individuals.
Diagnosis
- The CSF Cryptococcal Antigen test is the most sensitive for diagnosis. Induction therapy is with a combination of Amphotericin B or Liposomal Amphotericin B plus Flucytosine, followed by consolidation and maintenance therapy with Fluconazole.
- Persistent elevated intracranial pressure requires serial lumbar punctures or placement of an external ventricular drain.
- Candida meningitis affects the nervous system of immunocompromised individuals, especially those who are neutropenic. It occurs secondary to neurosurgical complications or due to infection of a VP shunt. CSF culture and CSF 1,3-β-D-glucan are frequently positive and help in diagnosis.
- Other aetiology of fungal meningitis depending on geographical location include Histoplasmosis, Blastomycosis, Coccidioidomycosis and Sporotrichosis.
Other causes of chronic bacterial meningitis
Lyme disease
- Lyme disease is caused by Borrelia burgdorferi and is spread via tick bites.
- The classic rash (erythema chronicum migrans) may or may not be noticed.
- Serology is useful for confirming the diagnosis.
- Both I/V ceftriaxone and oral doxycycline are effective in treating this condition.
Subacute meningitis syndrome
- Meningovascular syphilis refers to a subacute meningitis syndrome caused by the spirochaete Treponema pallidum.
- It should be ruled out in patients with HIV or in those with a history of sexually transmitted diseases.
- The CSF-VDRL test is specific for syphilis but has a low sensitivity.
- CSF FTA-ABS should be performed in negative cases with a high risk of suspicion.
- High-dose penicillin or ceftriaxone is the drug of choice for treatment.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Annesh Bhattacharjee is a Consultant Neurologist, at Dept. of Neurology GNRC Hospital, Guwahati.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries