Managing UTI in Paediatric Patients
M3 India Newsdesk Apr 02, 2024
This article guides diagnosing and managing urinary tract infections (UTIs) in children. It also emphasises proper evaluation methods, treatment with antibiotics, and long-term monitoring to prevent complications such as renal scarring and hypertension.
Introduction
Urinary tract infection (UTI) is a common bacterial infection in young children. Acute urinary tract infections are relatively common in children, with 8% of girls and 2% of boys having at least one episode by seven years of age. The most common pathogen is Escherichia coli, accounting for approximately 85 % of urinary tract infections in children.
Renal parenchymal defects are present in 3 to 15 % of children within one to two years of their first diagnosed urinary tract infection. Children < 1 year of age should be investigated after their first febrile UTI with a renal/bladder ultrasound to identify any significant renal abnormalities.
or children experiencing their first UTI, a voiding cystourethrogram is not necessary unless the results of the renal/bladder ultrasonography indicate a possible diagnosis of obstructive uropathy, specific renal abnormalities, or vesicoureteral reflux (VUR).
Incidence and prevalence of UTI
- In a 2008 systematic review, approximately 7% of children 2 to 24 months of age presenting with fever without a source and 8% of children 2 to 19 years of age presenting with possible urinary symptoms were diagnosed with a UTI.
- Long-term follow-up data are limited, although one Swedish study found that among patients who had renal scarring from pyelonephritis during childhood, 23% developed hypertension and 10% developed end-stage renal disease.
- However, more recent studies question the association between pyelonephritis and end-stage renal disease. Baseline abnormalities of the urogenital tract have been reported in up to 3.2% of healthy, screened infants.
- Additionally, obstructive anomalies are found in up to 4% and vesicoureteral reflux in 8 to 40% of children being evaluated for their first UTI. Compared to older children, children under the age of two may be more susceptible to parenchymal abnormalities.
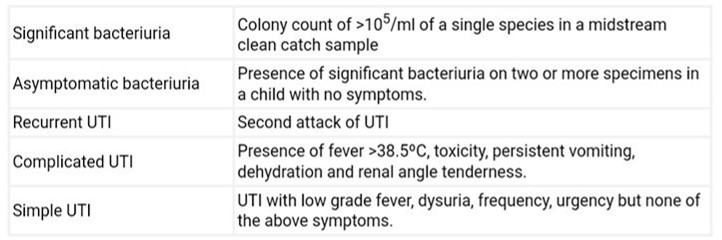
Definition
UTI is defined as an infection of the urinary tract identified by the growth of a significant number of organisms of a single species in the urine, in the presence of symptoms. When assessing and treating children who have UTIs, certain terminology is frequently utilised.
They are as follows:
Diagnosis of UTI in children
UTI may present as a simple viral fever in some infants and clinical features related to the urinary tract may not be present.
Diagnosis of UTI in young children is made in the presence of:
- Symptoms such as fever, dysuria, urgency, frequency, abdominal/flank pain in older children and fever, vomiting, diarrhoea, and poor weight gain in infants PLUS
- Positive dipstick for leukocyte esterase and nitrite (as a screening tool)
- Abnormal urinalysis with significant pyuria and bacteriuria AND
- Isolation of a single species of microorganism in significant numbers in a properly collected urine sample before starting antimicrobial therapy and testing for urine culture (gold standard)
Asymptomatic bacteriuria is considered in the presence of:
- Significant bacteriuria in the absence of pyuria or symptoms
- More common in girls compared to boys
- Often associated with nonvirulent Escherichia coli colonisation
- Ideally should not be treated with unnecessary antimicrobials
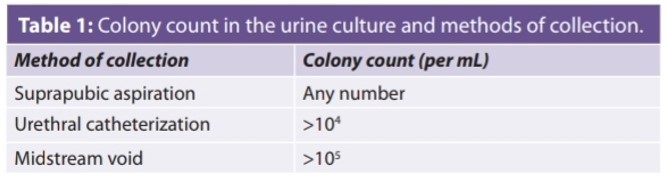
Significant bacteriuria: It is based on the colony count in the urine culture and method of collection (Table 1)
Ideal sample of urine for urine culture for diagnosis of UTI in young children:
- Toilet-trained children: Midstream collected urine by clean catch method (most preferred, non-invasive practical method). The genital area should be cleaned properly with soap and water before collecting a midstream urine sample.
- Non-toilet-trained children: Simple urethral catheterization OR Suprapubic aspiration.
Risk factors for UTI in young children (look for the presence of any of these in your patient):
- Poor perineal hygiene and unnecessary use of diapers.
- Congenital anomalies of the kidney and urinary tract (CAKUT) such as vesicoureteric reflux, pelvic ureteric junction obstruction, obstructive uropathy, abnormal communication between the urinary tract and gastrointestinal tract, phimosis in boys, vulval synechiae in girls, and renal stones.
- Bowel bladder dysfunction (BBD) presents with features of urinary urgency, frequency, dysuria, voiding postponement during the toilet training age group, incontinence, and constipation.
- Almost 50% of children with recurrent UTI and 10% of children presenting with a single UTI have an associated urological abnormality.
- Fungal UTIs are more common in immunocompromised patients, intensive care unit (ICU) settings, prolonged antibiotic usage, and in the presence of indwelling catheters.
Common organisms causing UTI are:
- E. Coli in >70% of cases
- Uncommon organisms—non-E. Coli bacteria like Klebsiella, Proteus, Enterobacter, Citrobacter, Staphylococcus saprophyticus, Enterococcus and fungi
Treatment of UTI in children
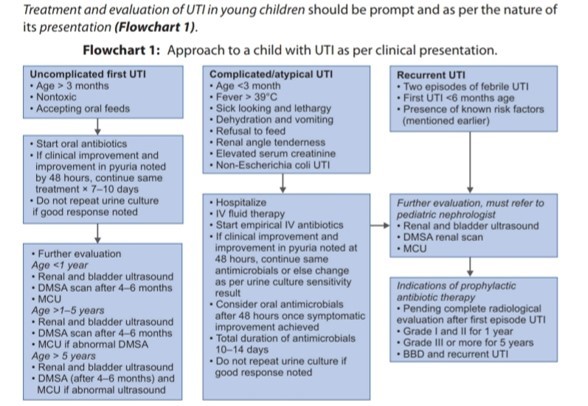
Antibiotics for UTI
- Therapy should be started after obtaining a urine culture
- Children with complicated UTIs and infants less than 3 months of age are treated with parenteral antibiotics.
- A combination of ampicillin and gentamicin, or a third-generation cephalosporin (cefotaxime or ceftriaxone) is preferred. When an infant is older than three to six months old, gentamicin may be given as a single medication. Once the child shows clinical improvement, with resolution of fever and toxicity, antibiotics may be administered orally. For the duration of treatment, parenteral antibiotics should be administered to children who have a positive blood culture and young newborns (less than three months old).
- For children older than three months who have an uncomplicated UTI, oral medicines are prescribed.
- Amoxicillin, cotrimoxazole or an oral cephalosporin is preferred.
- Quinolones should be avoided as first-line medication; their use is guided by results of urine sensitivity.
- Since nitrofurantoin and nalidixic acid do not reach therapeutic quantities in the circulation or renal parenchyma, they should not be used to treat UTIs.
- Patients who do not exhibit clinical response (reduction of fever and toxicity) after 48 hours of the start of treatment require an abdominal ultrasonography and a repeat urine culture.
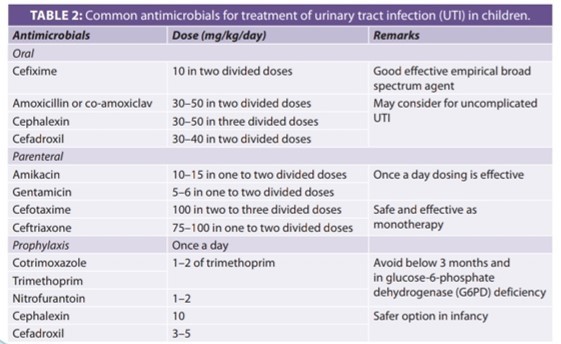
Common antimicrobials for the treatment of UTI in children are presented in Table 2
Antibiotic prophylaxis
Long-term, low-dose, antibacterial prophylaxis is used to prevent recurrent febrile UTIs. The ideal antibiotic used should be effective, and non-toxic with few side effects and not alter the indigenous bacterial flora or induce the development of bacterial resistance. Medications used for prophylaxis are given as a signal bedtime dose.
Antibiotic prophylaxis is recommended under the following circumstances:
- Following treatment of: (i) the first UTI in all children below 2 years of age, and (ii) complicated UTI in children below 5 years old, while awaiting imaging studies.
- Children with VUR.
- Patients show renal scars following a UTI even if reflux is not demonstrated. Prophylaxis may be stopped if a radionuclide cystogram or MCU repeated 6 months later is normal.
- Children with frequent febrile UTI (3 or more episodes in a year) even if the urinary tract is normal.
Further follow-up and monitoring
- Aim for symptomatic improvement, complete and sustained resolution of fever, and return to normal well-being
- After the current UTI treatment, record a normal urine analysis
- Urine cultures should not be repeated unless a new or breakthrough UTI is present
- Periodic monitoring of growth
- Urine analysis during further febrile episodes in the presence of a known risk factor for UTI
- Blood pressure evaluation once in 6–12 months
- Assess renal function once a year in a child who has severe complicated UTI or recurrent UTI
- Be aware of proteinuria. It may be linked to pyelonephritic kidney scarring following successful UTI treatment, necessitating medical intervention.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Shaukat Panjawani is a Consultant Paediatrician and Neonatologist at Olive Multispecialty Hospital, Vapi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries