Management of Neuropathic Pain
M3 India Newsdesk Aug 09, 2023
Neuropathic pain is typically caused by persistent, degenerative nerve illness, however, it can also be caused by an injury or infection. This article explains the types and causes of neuropathic pain along with its treatments including nonpharmacologic therapies.
Neuropathic pain (NP)
Neuropathic pain is caused by damage to or dysfunction of the nerves, spinal cord, or brain. Depending on the site of the lesion NP can be:
- Central NP: Occurs when the dysfunction affects the central nervous system e.g.- Central post-stroke pain, Spinal cord injury pain.
- Peripheral NP: Occurs when the dysfunction affects the peripheral nervous system e.g. - Radicular pain, Diabetic Peripheral Neuropathy (DPN), Infections like Postherpetic neuralgia (PHN), HIV-related neuropathies, Cancer-related NP.
Major types of pain
- Nociceptive Pain: Caused by an injury to body tissues
- Psychogenic Pain: Pain that is mostly related to psychological factors
- Neuropathic Pain: Caused by damage to or dysfunction of the nerves, spinal cord, or brain
Causes of neuropathic pain
- Diabetic peripheral neuropathy: The most common complication and greatest source of morbidity in diabetes patients. DPN manifest in the following forms: Peripheral sensorimotor polyneuropathy and Autonomic neuropathy.
- NP in Low back pain (LBP): Common causes of LBP are Disc prolapse (33.4%), Lumbar Spondylosis (26.9%), Spinal canal stenosis (10.6%), Spinal cord injury (7.1%).
- Postherpetic neuralgia (PHN): With a resolution of the HZ eruption, pain that continues for 3 months or more is defined as PHN. PHN is a complication of herpes zoster.
- HIV-Associated Peripheral Neuropathy: Due to HIV infection itself, Due to some HIV treatment-related toxicity Nucleoside reverse transcriptase inhibitors (NRTIs)—are potentially neurotoxic E.g. stavudine, didanosine, and zalcitabine.
- Pain in Cancer Patients: Due to compression/infiltration produced by cancer in the nervous system and due to compression/infiltration produced by cancer in the nervous system.
- Central post-stroke pain: The patient experiences constant or intermittent pain on the affected side of the body with associated sensory abnormalities.
- NP After Spinal Cord Injury (SCI): At the level of the SCI, in a segmental pattern and three segments below the level of injury.
Nonpharmacologic therapies
Nonpharmacologic therapies encompass a wide array of treatments that may be grouped into exercise therapy, psych-educational interventions (eg, cognitive-behavioural therapy [CBT], family therapy, psychotherapy, and patient education), mind-body therapies (eg, mindfulness-based stress reduction [MBSR]), and physical interventions (eg, including physical therapy [PT], acupuncture, chiropractic manipulation, massage, and others).
Commonly used drugs in the Management of Neuropathic Pain

Antiseizure medications
They are the 1st line drugs: Gabapentin and Pregabalin they bind to voltage-gated calcium channels producing changes in neurotransmitter release. Pregabalin can be started with 75/150 mg per day and can be increased to a maximum of 300 mg/day, 600 mg/day within 1 week. Duration of treatment depends on the response of individual patients to the treatment and the cause of NP Avg. duration in the clinical trials -8 to 12 weeks.
Treatment with gabapentin should be initiated at a low dose with gradual increases until pain relief or dose-limiting adverse effects are achieved. Gabapentin is typically initiated at 300 mg at night.
The typical effective daily dose range for immediate-release (IR) gabapentin is 1200 to 2400 mg/day on a three-times-a-day schedule, with a maximum daily dose of 3600 mg.
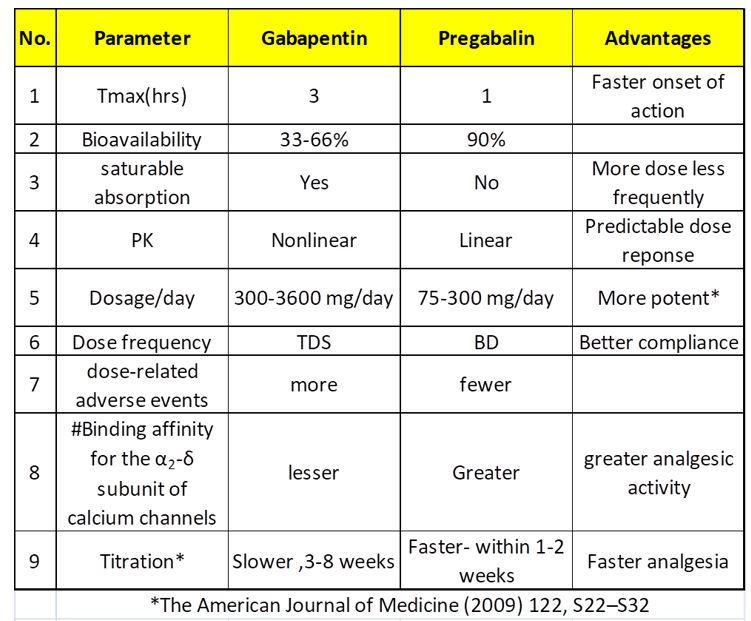
Comparison of gabapentin and pregabalin
Tricyclic antidepressants: Amitriptyline has been the most widely studied TCA in chronic pain; others including doxepin, imipramine, nortriptyline, and desipramine also have been used effectively. Nortriptyline may be started at 10 mg/day orally, increasing the dose at weekly intervals in 10 to 25 mg increments based on response.
Serotonin-norepinephrine reuptake inhibitors: venlafaxine and duloxetine have been used for the treatment of peripheral neuropathic pain, and duloxetine and milnacipran have been used for the treatment of fibromyalgia. Duloxetine is approved by the FDA for the treatment of major depression, anxiety, and stress urinary incontinence. Side effects include nausea, dry mouth, insomnia, drowsiness, constipation, fatigue, and dizziness.
Topical agents: Topical NSAIDs, in the form of a gel, spray, or cream, can provide relief for acute musculoskeletal pain. Topical lidocaine is considered second-line therapy for some forms of neuropathic pain. Topical Capsaicin has been used in patients with post-herpetic neuralgia, HIV neuropathy, diabetic neuropathy, and patients with osteoarthritis in one or a few joints.
Botulinum toxin: Limited literature suggests that subcutaneous injection of botulinum toxin type A (BTX-A), a potent neurotoxin, may reduce the opioid requirement for analgesia in patients with severe post-herpetic neuralgia.
Opioids: Long-term opioids should not routinely be used for chronic pain. If opioids are necessary, they should be used at the lowest effective dose. Tramadol may be used as a second-line agent for patients with fibromyalgia who have not responded to initial therapy with other agents. Tapentadol is the only opioid with a specific US Food and Drug Administration (FDA) indication for neuropathic pain (ER form for painful diabetic neuropathy). For chronic pain indications, buprenorphine is available as a transdermal patch or a buccal film.
Effective treatment of pain requires multimodal analgesia with an emphasis on non-drug modalities (eg, self-management, behavioural health support and physical therapy). When necessary, we add multi-targeted pharmacologic therapies.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Nikhil Repaka is a Neuro physician at Jagruth Super Specialty Hospital, Khammam.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries