Making Decisions in Medical Practice on Acute Abdominal Pain
M3 India Newsdesk Mar 06, 2024
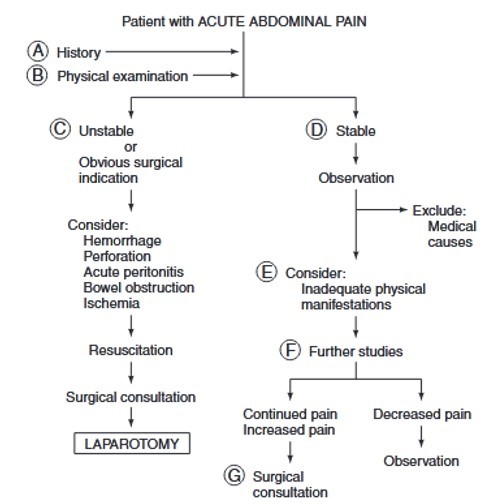
In cases of acute abdominal pain, prompt evaluation through history and physical examination is crucial. Surgical consultation should be considered early, especially for severe pain lasting over six hours, while various investigations, including imaging, help in narrowing down potential causes.
In the emergency room and primary care context, acute abdominal discomfort is often seen as a clinical presentation.
The optimum course of action for a physician treating a patient presenting with acute abdominal pain would be to rule out acute medical reasons for the pain and determine when surgery is best advised. The bar for engaging surgical competence should be low.
Evaluation requires a thorough history and physical examination. It is customary to seek admission for assessment when there is severe pain that lasts for more than six hours and there is no clear surgical justification. Visceral, parietal, and transferred abdominal discomfort are all possible.
The ventral midline of the abdomen experiences dull, often poorly localised pain when noxious stimulus affects the abdominal viscera. The damaged organs' multisegmental innervation explains this. Pain that is more localised and often more intense is caused by irritation of the parietal peritoneum.
Finally, since these locations have the same segmental innervation as the affected organ, referred pain is felt in distant places from the site of damage.
Start with history and examination
The differential diagnosis may be narrowed with a thorough history.
Sex and age are significant factors. Younger people get mesenteric adenitis, whereas older people have vascular and neoplastic diseases. Think about pelvic inflammatory illness or ectopic pregnancy in a sexually active female.
Past medical histories may include-
- Gallstones
- Diverticular disease
- Inflammatory bowel disease
- Stomach surgery
- Peptic ulcer disease
Medication history may reveal the usage of immunosuppressants or corticosteroids. Diabetes mellitus and other coexisting medical disorders may have an impact on the presentation.
It matters how the pain starts and what kind of discomfort it is. As with intestinal perforations, peritonitis is suggested by an abrupt onset of severe, localised, "somatic" pain.
Colic or gradually worsening "visceral" discomfort is more indicative of ureteral, cystic duct, or colon blockage. A changing pattern of pain, first visceral and then somatic, might indicate cholecystitis, appendicitis, or strangulation of the colon.
Ischemia causes disproportionate pain concerning a less severe physical finding. Radiation patterns specific to pancreatitis (back), appendicitis (lower right quadrant), and cholecystitis (scapula) are seen.
Before the examination, observe the patient for:
Movement and restlessness: Parietal pain worsens with movement, while visceral discomfort often leads to restlessness.
Auscultation: Check the abdomen for bowel sounds, bruits, and rubs.
Palpation technique: Begin palpation a distance from the painful location.
- Peritonitis signs: Involuntary guarding or rebound soreness, especially with modest percussion.
- Deeper palpation: Detect organomegaly or masses with deeper palpation.
Pelvic and rectal exams: Conduct thorough pelvic and rectal examinations.
External genitalia and hernial orifices: Examine the external genitalia as directed, and check for hernias in the groin.
Initial management
Urgent surgical considerations
- An urgent laparotomy may be necessary for a patient who is hemodynamically unstable and may be experiencing intraabdominal bleeding.
- In addition, the patient should receive an emergency surgical assessment if they have hypotension, a high temperature, leukocytosis, and suspicious physical examination findings (involuntary guarding, stiffness, and growing severe soreness).
- A surgical evaluation is necessary for suspected intestinal ischemia accompanied by acidosis, fever, and hypovolemia.
- Additionally, patients who exhibit perforation evidence by plain radiography, contrast studies, or paracentesis should be investigated.
Pre-examination resuscitation
- Before and throughout further examination, resuscitation is essential. This includes IV access and fluids for ventilatory support, nasogastric suction, oxygen, and urine output monitoring.
- Frequent vital sign checks and initial laboratory testing should also be performed.
- Ideally, urinalysis, electrocardiography, and abdominal films may be used to rule out significant medical reasons for acute discomfort prior to surgery.
Watching the course of symptoms
It is important to keep a careful eye on the patient who is more stable. Acute abdominal discomfort may have many medical reasons, but many of them can be ruled out.
- The most frequent causes include mesenteric adenitis, pyelonephritis, and acute pneumonitis, particularly in the lower lobe.
- Perforation may result from collagen vascular disease. Abdominal discomfort may be a symptom of many metabolic illnesses, such as acute intermittent porphyria, Addisonian crisis, diabetic ketoacidosis, and uremia.
- A history of ascites and chronic liver illness may indicate spontaneous bacterial peritonitis.
There are certain people who may appear with a disparity in the physical findings and the severity of their illness. These include people who are immunocompromised, aged, malnourished, fat, on steroids, or who are in the early stages of recovery after surgery; they also include patients who have altered mental states and paraplegic patients.
Investigations to be checked
- Laboratory examination
- Haemoglobin/hematocrit
- White blood cell count
- Differential
- Electrolytes
- Blood gases
- Amylase
- Liver tests
- Coagulation times
- Urinalysis
- Every woman who is of reproductive age must get a serum pregnancy test.
- Abdominal films taken while supine or upright may indicate the presence of renal calculi, ischemia, blockage, perforation, or intraabdominal abscess.
- Additionally useful in determining possible thoracic sources of transferred pain is a chest X-ray investigation.
- When ischemia or bleeding is suspected, angiography might be helpful.
- Studies using contrast are helpful when a perforation is suspected.
- Pancreatitis, cholecystitis, an abscess, a retroperitoneal tumour, or a dilated biliary tree may all be seen on ultrasound and CT imaging.
- The CT scan is very effective in diagnosing a wide range of abdominal discomfort reasons. For instance, it has been found to have a sensitivity of 98% and specificity of 97% for the diagnosis of appendicitis.
- Ultrasonography has been shown to have comparable diagnostic accuracy and may be used as a first line of investigation for pain that may have a hepatobiliary cause.
Analysing closely can reveal an evolutionary trend in the abdominal pain condition. If you haven't already, get a surgical consultation if the intense discomfort lasts more than six hours.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries