Magnetic sphincter augmentation better than PPIs for intractable GERD
M3 Global Newsdesk Sep 10, 2018
Among patients with gastroesophageal reflux disease (GERD), nearly 90% who underwent laparoscopic magnetic sphincter augmentation (MSA) reported relief of regurgitation, compared with 10% of patients on twice-daily proton pump inhibitors (PPIs), according to a new study in Gastrointestinal Endoscopy.
“Treating GERD surgically corrects the sphincter defects and significantly reduces the number of reflux events, rather than merely reducing the acidity of the refluxate,” wrote lead author Reginald Bell, MD, Institute of Esophageal and Reflux Surgery, Englewood, CO, and coauthors. “It is therefore extremely effective at controlling regurgitative symptoms.”
Although PPIs reduce gastric acid secretion—thus soothing heartburn and helping with esophagitis—they do not alter lower esophageal sphincter (LES) function or mitigate regurgitation. Nevertheless, physicians commonly continue to treat complaints of persistent regurgitation by increasing doses of PPIs, even in patients who are refractory to these drugs.
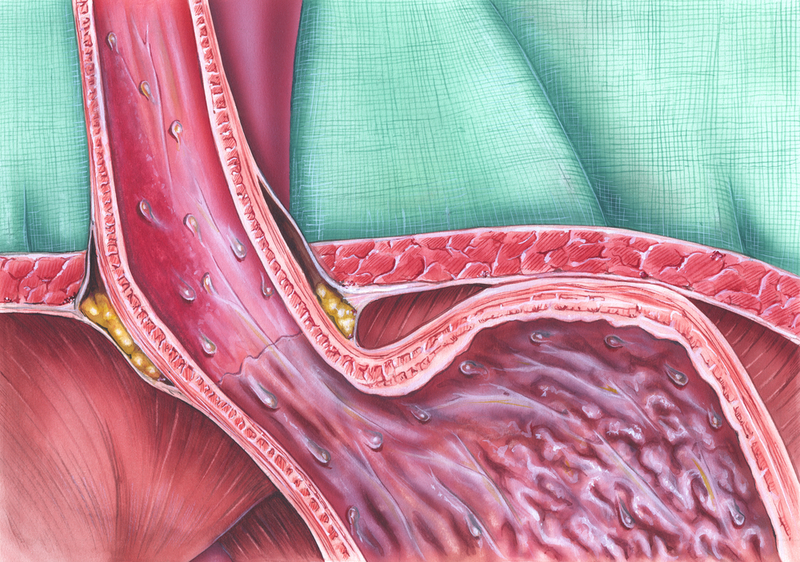
MSA consists of a “bracelet” of magnetic beads laparoscopically placed at the level of the distal esophagus. This string of beads aids LES function by separating during pressure caused by swallowing; however, most GERD events transpire at pressures too low to open the augmented sphincter. Previous single-arm studies have shown that MSA is both safe and effective at controlling symptoms of GERD, including heartburn and regurgitation.
For this study, the researchers recruited 152 adult GERD patients with moderate-to-severe regurgitation that was refractory to 8 weeks of once-daily PPI treatment. The team randomized 50 patients to laparoscopic MSA and 102 patients to twice-daily (BID) PPI therapy with omeprazole 20 mg.
At baseline and 6 months, the team administered standard symptom questionnaires and quality of life surveys, and performed ambulatory esophageal reflux monitoring. At 6 months, patients in the BID PPI arm could crossover to the MSA arm and then undergo further evaluation at 12 months.
At 6 months, 89% of patients in the MSA arm reported regurgitation relief compared with 10% of patients in the BID PPI arm (P <0.001). On intention-to-treat analysis, these findings attenuated to 84% of MSA patients and 10% of BID PPI patients (P <0.001).
With respect to health-related quality of life scores, 81% of patients in the MSA arm experienced more than 50% global improvement as compared with 8% of BID PPI patients (P <0.001). Notably, 92% of MSA patients ended up discontinuing PPIs.
Overall, MSA patients experienced substantially fewer reflux events than did BID PPI patients, as measured by impedance-pH testing. Specifically 91% of MSA patients evidenced a normal number of reflux events at 6 months, and 89% evidenced normal esophageal acid exposure.
“This study demonstrates that control of reflux events (by MSA) is more important than neutralization of gastric pH (as occurs with PPI therapy) in controlling regurgitative symptoms,” the authors wrote.
Researchers observed no notable safety concerns in the current study, although 28% of MSA patients reported transient dysphagia, with 4% of patients complaining of ongoing dysphagia.
Dr. Bell and colleagues noted that capsular formation, or scarring, is expected after any implantation, including MSA. The researchers suggested that patients regularly ingest semisolid boluses 2-4 weeks postoperatively to minimize the risk of scarring and chronic dysphagia. Also, some MSA patients may benefit from a short course of steroids.
The investigators conceded that one potential limitation of the current study was that subjective questionnaires were employed to analyze most endpoints.
“Magnetic sphincter augmentation provides significantly better control of moderate-to-severe regurgitation when compared with BID PPI therapy,” the authors concluded. “GERD patients whose regurgitation is inadequately controlled after initial dosing of acid-suppressive medication should be considered for minimally invasive surgical treatment with the MSA rather than treated with increased dosing of medication.”
This story is contributed by Naveed Saleh and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries