A Comprehensive Guide to Liver Transplants: Decoding the 5 'W' Questions
M3 India Newsdesk Nov 24, 2023
Liver transplants replace a diseased liver with a healthy one to treat end-stage liver disease or cancer. This article summarises key aspects, including the need, candidate criteria, transplant types, timing, & the impact of centre volume on outcomes.
In India, all forms of liver failure were the eighth leading cause of death in 2020. Liver failure disproportionately affects men in the peak of their productive years (3rd and 4th decade). Often, liver transplantation (LT) remains the only curative treatment for such patients with end-stage liver disease or liver cancer. Hence the importance of referral for LT at the appropriate time is of paramount importance. Unfortunately, the lack of awareness often leads to very late and in several instances absence of referral for transplantation.
This article outlines the importance of LT in improving the patient's quality of life and decreasing the morbidity and mortality related to acute and chronic end-stage liver disease. It highlights the indications, contraindications, and the liver transplantation technique.
Why do we need liver transplantation?
The liver has a unique capacity among organs to regenerate itself after damage. A liver can regrow to a normal size even after up to 90% of it has been removed. But the liver isn’t invincible. Beyond a certain threshold, acute and chronic forms of liver injury clinically manifest with signs of liver failure. Chronic liver disease, or cirrhosis, is also a risk factor for the development of hepatocellular carcinoma (HCC).
Although, in certain situations, it is possible to reverse cirrhosis with currently available therapies targeting the underlying disease, it remains a rare occurrence. Current therapeutic options for many underlying diseases are suboptimal, and effective therapies targeting liver fibrosis are absent. Additionally, there are no effective organ replacement therapies for the liver, such as dialysis or ventricular assist devices for the kidney or heart respectively
Patients with severe acute failure or decompensated advanced chronic liver disease are hence invariably left with liver transplantation as the last hope. Liver transplantation can effectively cure liver failure, cancer, or metabolic liver diseases. Reported rates of post-transplant survival in India range from 64-88% and are par with internationally reported outcomes. A successful LT, on average, extends its lifespan by 15 years. Hence, liver transplantation should be discussed as a definitive therapy wherever indicated.
Who should be considered for liver transplantation?
According to the AASLD-AST Evaluation for Liver Transplantation Guidelines 2013, a liver transplant is indicated when the limits of medical therapy have been reached.
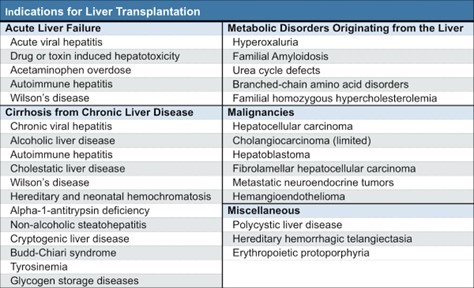
It further outlines four major types of indications for liver transplantation:
- Acute liver failure
- Complications of cirrhosis
- Liver-based metabolic diseases
- Systemic complications of chronic liver disease
In addition, there are some rare conditions that can warrant liver transplantation.
In addition to the above-established indications, data is now emerging about the effectiveness of liver transplantation in severe alcoholic hepatitis, acute on chronic liver failure and selected cases of liver metastases from either colorectal carcinoma or neuroendocrine tumours. However, these are not routine indications and decision is usually taken on a case-by-case basis.
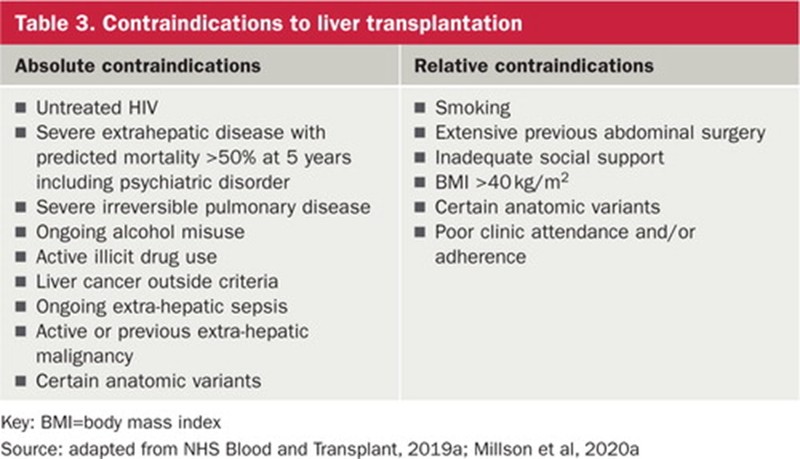
Contraindications
What are the different types of liver transplantation?
Liver transplantation can be classified in various ways depending on the urgency of the clinical situation, the types of liver donors, and the site of implantation.
Most liver transplants are elective, except in the setting of acute liver failure, where an emergency liver transplant is often needed
Donor type
Deceased donor liver transplant – liver allograft is harvested from a deceased donor by performing a complete hepatectomy. Traditionally this type of transplant involves organ donated after brain death (DBD). In the West, increasingly organs donated after cardiac death (DCD) are being used to overcome organ demand.
Spit-liver transplant – a single deceased donor liver allograft is divided into right and left portions that are implanted into two recipients simultaneously. Typically, an adult patient receives about 60 per cent of the liver (the right lobe), while a pediatric patient receives the other about 40 per cent of the liver (the left lobe).
Living donor liver transplant: Liver allograft is harvested from a living donor by performing a partial hepatectomy. Allografts can be the entire right or left liver lobe or sometimes just left lateral segments
ABO-incompatible liver transplant – liver allograft is harvested from a living donor with an incompatible blood group. The recipient is conditioned to receive the graft using advanced immunosuppression protocols to bring down antibody levels below a permissible limit before transplant to prevent organ rejection. In small children, the antibody levels are very low and ABOi transplant can be performed with less preparation and better success.
Swap liver transplant – When one of the patient’s family members is suitable and willing for donation, but is not a good match for the patient, a paired donation or swap transplant may be considered. In this type of transplant, two families with suitable living donors exchange their donors because they are not a good match for their own patients, but are appropriate for each other’s patients.
Dual lobe liver transplant – When a potential living donor’s liver volume is found inadequate for the recipient on a pre-operative CT scan, he/she may be rejected. It is common that in one family, two or more people, who were otherwise suitable, might have been rejected for donation because of low liver volumes. If partial livers from both are combined, it is often adequate for the patient. In such a transplant, three operations (one recipient and two donors) are performed simultaneously.
Domino liver transplant: A domino (or sequential) liver transplant involves three patients: one deceased liver donor, one living liver donor/recipient and one liver recipient. In most cases, a young patient with a metabolic disorder (such as amyloidosis) receives a liver from a deceased donor. The young patient's liver is then harvested for donation to an older patient with end-stage liver disease. The success of this "domino" procedure is based on the expectation that the older recipient will not experience symptoms of the metabolic disorder, which could take decades to be symptomatic.
Site of implantation
Orthotopic – native liver is removed completely and allograft (whole liver or partial liver) is implanted in its place
Heterotopic transplant – allograft is implanted in the abdomen while the recipient's native liver remains in place.
Auxiliary liver transplant
The whole or part of the native liver is left behind and the liver allograft is implanted in either orthotopic or heterotopic position. The principle of auxiliary liver transplantation is the implantation of a right or left hemiliver into the abdominal cavity to restore normal liver function temporarily, while the native liver recuperates. Once the native liver has recovered, the graft can be removed or left in place without immunosuppression leading to atrophy.
When is the right time to do a liver transplant?
The timing of liver transplantation is dependent on underlying indications.
Decompensated chronic liver disease
This is the most common indication for liver transplantation. Decompensation is defined by the occurrence of a complication, such as ascites, variceal bleeding, hepatic encephalopathy, spontaneous bacterial peritonitis, or hepatorenal syndrome. The development of decompensated cirrhosis negatively influences the prognosis. In a natural history study of persons with cirrhosis, more than 90% with compensated cirrhosis were still alive after 5 years, compared with only 50% survival at 5 years among those who experienced a decompensating event. Moreover, once decompensation occurred, 20% died within one year. Accordingly, people with cirrhosis should be referred for transplant evaluation when they experience their first major cirrhosis-related complication, such as ascites, variceal bleeding, or hepatic encephalopathy.
In India, prioritisation in the transplant list is done based on the MELD-Na score. Based on current guidelines, individuals with a MELD- Na score of 15 or greater should be referred to a liver transplant centre for evaluation. Certain complications of cirrhosis, like porto-pulmonary hypertension, hepatopulmonary syndrome, and hepatocellular carcinoma, are given MELD exception points to truly reflect the severity of the disease and clinical urgency.
Acute liver failure
Acute liver failure is defined by the presence of coagulopathy (INR ≥ 1.5) and hepatic encephalopathy, presenting within 26 weeks from the onset of symptoms, without preexisting liver disease. Listing for liver transplantation in ALF usually is based on the original or modified King’s College and Clichy criteria.
Liver cancer
The Milan criteria (1 lesion > 2 cm and ≤ 5 cm, or up to 3 lesions, each ≥ 1 cm and less than or ≤ 3 cm, no macrovascular involvement) have been adopted by many transplant societies worldwide as the criteria to determine whether patients with HCC can move forward with liver transplant
Where should the transplant be performed?
The relationship between transplant centre volume and patient outcomes has been reported in multiple studies. However, there is no clear minimal threshold volume. Generally, centres performing 60-80 transplants per year are considered high volume and reported to have better outcomes whereas centres with less than 20 transplants per year have relatively lower survival and higher mortality rates.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Parag Dashatwar is a DNB gastroenterologist, leading the department of medical gastroenterology at Olive Hospital, Hyderabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries