Infectious Diseases Commonly Seen in HIV Patients
M3 India Newsdesk Apr 06, 2023
Human immunodeficiency virus (HIV) is a blood-borne virus typically transmitted via sexual intercourse, shared intravenous infected needles, and during the birth process or via human milk (vertical transmission). This article discusses the classification and aetiology of HIV-related infections.
Infectious diseases in HIV patients
HIV presently accounts for the highest number of deaths attributable to any single infective agent. The number of People Living with HIV (PLHIV) in India is estimated at around 24 lakhs in 2021. The threat to their life is not from the virus alone.
Opportunistic infections (OIs) and associated complications account for a considerable proportion of such morbidity & mortality. Appropriate and timely management of OIs is as important as antiretroviral therapy (ART) in preventing mortality and morbidity among HIV-infected persons.
Aetiology
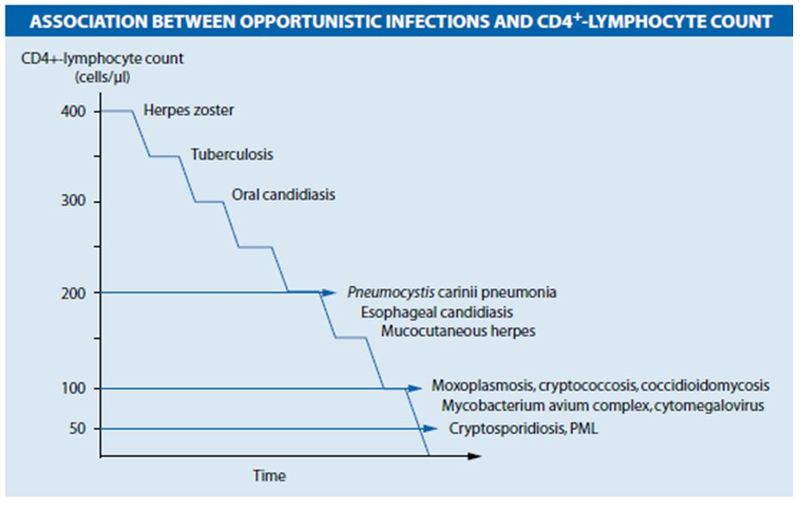
Human immunodeficiency virus (HIV) is a retrovirus known to attack the CD4+ T lymphocytes. HIV-infected individuals, even with high CD4+ cell counts, are at a higher risk of developing both common and OIs than the general population. However, in HIV patients with CD4+ cell counts less than 200 cells/mm, the risk of developing OIs and subsequent death remains the highest.
Figure 1. shows the association between CD4+ cell counts and common infections.
Classification
HIV-related infections are divided into the following categories:
- Bacterial infections- Tuberculosis, Respiratory infections, Enteric infections, Atypical mycobacteriosis, Bartonellosis.
- Fungal infections- Candidiasis, Cryptococcosis, Histoplasmosis, Pneumocystis jirovecii pneumonia (PCP), Coccidioidomycosis.
- Viral infections- Herpes simplex virus (HSV), Varicella-zoster virus (VZV), Cytomegalovirus (CMV), Human herpesvirus 8 (HHV8) infection, Human papillomavirus (HPV) infection, Progressive multifocal leukoencephalopathy, Hepatitis B and C.
- Parasitic infections- Toxoplasmosis, Cryptosporidiosis, Microsporidiosis, Isosporiasis, Leishmaniasis.
Clinical features and management of different OIs in HIV patients
Tuberculosis (TB)
- Tuberculosis (TB) caused by a bacterium called Mycobacterium tuberculosis is the leading HIV-associated opportunistic disease in developing countries.
- TB can spread through the air when a person with TB coughs, sneezes or speaks.
- Symptoms of TB in the lungs include cough, tiredness, weight loss, fever, and night sweats.
- The DOTS (directly observed, short course) treatment strategy recommended by WHO to treat TB in HIV-infected persons.
Mycobacterium Avium Complex (MAC)
- MAC is caused by infection with different types of mycobacterium: Mycobacterium avium, Mycobacterium intracellulare, or Mycobacterium kansasii.
- Symptoms include fever, weight loss, night sweats, diarrhoea, and wasting.
- Infections with these bacteria spread throughout the body and can be life-threatening in people with weakened immune systems.
Pneumonia
- Lower respiratory tract infections are the most common recurrent infections in PLHIV. They are usually life-threatening and can be caused by bacteria, viruses and fungi.
- HIV patients appear to be particularly prone to infections with encapsulated organisms such as Streptococcus pneumoniae and Haemophilus influenza.
- The diagnosis of pneumonia is usually made on clinical grounds and by a chest X-ray, or sputum examination.
- People with HIV should get a vaccine to prevent infection with streptococcus pneumoniae.
Candidiasis
- Candidiasis is caused by an infection with a fungus called Candida.
- The two main types of candidiasis are localised disease (of the mouth and throat, and of the vagina), and systemic disease (of the oesophagus, and disseminated disease).
- The symptom of oesophageal candidiasis is difficulty and pain during swallowing. Disseminated candidiasis causes fever and symptoms in the organs affected by the disease.
- A localised disease is treated first with topical drugs while Systemic candidiasis requires treatment with systemic antifungal agents such as ketoconazole itraconazole, fluconazole or amphotericin B.
Coccidioidomycosis
- This illness is caused by the fungus Coccidioides.
- It is sometimes called valley fever, desert fever, or San Joaquin Valley fever.
- People can get it by breathing in fungal spores.
- Four different syndromes are noted:
- Focal pneumonia
- Diffuse pneumonia
- Meningitis
- Positive serology tests without evidence of localised infection
Cryptococcosis
- Systemic mycoses such as cryptococcosis caused by infection with the fungus Cryptococcus neoformans probably cause 5% of all HIV-associated deaths worldwide.
- Cryptococcosis most often appears as meningitis, and occasionally as pulmonary or disseminated disease.
- Cryptococcal meningitis is the most frequent systemic fungal infection in HIV-infected persons, Fever, malaise, and headache are the common presenting symptoms.
- Cryptococcosis is relatively easy to diagnose by clinical signs and symptoms and CSF examination.
- Treatment is systemic antifungal like fluconazole, amphotericin b, and flucytosine.
Pneumocystis Pneumonia (PCP)
- PCP is the most frequent HIV-associated associated opportunistic infection in industrialised countries caused by the fungus Pneumocystis jirovecii.
- The symptoms are mainly pneumonia along with fever and respiratory symptoms such as dry cough, chest pain and progressive dyspnoea, hypoxemia.
- Definitive diagnosis requires microscopy of bodily tissues or fluids, chest x-ray, and bronchial leavage.
- Mild cases can be treated with oral TMP-SMZ. Severe cases of PCP are initially treated intravenously with TMP-SMZ, or clindamycin and oral primaquine along with Supportive therapy including oxygen.
- Prevention of PCP is strongly recommended for HIV-infected persons with significant immune compromise.
Histoplasmosis
- Histoplasmosis is caused by the fungus Histoplasma.
- Histoplasmosis most often develops in the lungs and produces symptoms similar to the flu or pneumonia.
- Severe disseminated histoplasmosis manifesting as fever, fatigue, cough, weight loss, lymphadenopathy, hepatosplenomegaly, and mucocutaneous ulcers of the nose, mouth, tongue, and intestine may occur.
- Diagnosis is made on clinical grounds and is confirmed by fungal cultures or histological examination of biopsied tissues.
Cytomegalovirus (CMV)
CMV can infect multiple parts of the body and cause pneumonia, gastroenteritis (CMV colitis), encephalitis (infection) of the brain, and sight-threatening retinitis (CMV retinitis).
Diagnosis- The most frequent localisation is the retina which is diagnosed by a specialised ophthalmologist. Other localisations require sophisticated equipment and costly tests, such as tissue biopsies and deoxyribonucleic acid (DNA) hybridisation studies.
Treatment- Treatment aims to alleviate symptoms, and prevent blindness, rather than provide a cure. The drugs currently used are ganciclovir and foscarnet.
Herpes Simplex Virus (HSV)
- Herpes simplex virus infection (HSV, which causes sores around the mouth and genitals) and herpes zoster virus infection (“zonal” herpes) are not life-threatening but can be extremely painful.
- In people with severely damaged immune systems, HSV can also cause infection of the bronchus, pneumonia, esophagitis, meningoencephalitis and meningitis which can be life-threatening.
- Treatment options are local as well as systemic antiviral therapy like acyclovir, valacyclovir, and gancyclovir.
Kaposi's Sarcoma (KS)
- KS is caused by a virus called Kaposi’s sarcoma herpes virus (KSHV) or human herpes virus 8 (HHV-8).
- HIV-associated Kaposi sarcoma causes dark blue lesions which can occur in a variety of locations including the skin, mucous membranes, gastrointestinal tract, lungs or lymph nodes.
- Treatment depends on the symptoms and location of the lesion.
- For local lesions, injection therapy with vinblastine, Radiotherapy can also be used, especially in hard-to-reach sites such as the inner mouth, eyes, face and soles of the feet. For severe widespread disease, systemic chemotherapy is the preferred treatment.
Progressive Multifocal Leukoencephalopathy
- This rare brain and spinal cord disease is caused by the JC (John Cunningham) virus mostly seen in severely immunocompromised patients.
- Symptoms may include paralysis, blindness, speech problems, and an altered mental state.
- This disease often progresses rapidly and may be fatal.
Toxoplasmosis
- This infection is caused by the parasite Toxoplasma gondii.
- The parasite is carried by warm-blooded animals including cats, rodents, and birds and is released in their faeces.
- Symptoms include altered mental status, fever, seizures, headaches, and focal neurological findings, including motor deficits, cranial nerve palsies, movement disorders, visual-field loss and aphasia.
- Diagnosis of toxoplasmosis is by CT scan or MRI scan.
- Serological tests for Toxoplasma antibody (immunoglobulin G, or IgG) may help in establishing the diagnosis in the absence of neuroimaging techniques.
- If toxoplasmosis is strongly suspected, patients are more likely to be given a trial of therapy.
Leishmaniasis
- Visceral leishmaniasis (VL) is a neglected vector-borne disease caused by Leishmania donovani parasite and is transmitted by infected sebotomus argentipes).
- The majority of the cases occur in five countries viz. India, Bangladesh, Sudan, Ethiopia and Brazil. Out of the worldwide VL cases, about 50% are reported from India alone, however, Bihar state contributes 80% of VL cases.
- The most serious of its four forms is visceral leishmaniasis(VL) also known as kala-azar which is characterised by irregular bouts of fever, substantial weight loss, swelling of the spleen and liver, and pancytopenia.
Case study 1
A 30-year-old male patient, presented with complaints of recurrent fever with chills for six months, progressive generalised weakness for five months and loss of appetite for one month. He was a known case of HIV on HAART for 5 years.
On general examination, the patient had moderate pallor, no icterus, cyanosis and lymphadenopathy. On abdominal examination, the liver was palpable about 2cm right below the costal margin and the spleen was palpable up to 7cm below the left costal margin Examination of the other systems was unremarkable.
Diagnosis
CBC revealed pancytopenia with HB-7g/dl, TLC-2700/μ, and platelets count 63000/ml. The peripheral blood smear was unremarkable, and other investigations like hepatitis B and C, cytomegalovirus, parvovirus B19, Epstein-Barr virus, Interferon-γ release assays, as well as Brucella, Coxiella burnetii, Rickettsia were all negative. Bone marrow smears revealed an abundance of amastigote forms of Leishmania donovani (also known as LD bodies) both intracellularly within the macrophages as well as extracellularly.
Treatment
Intravenous liposomal amphotericin- B was given as per the regimen of 3mg/kg/day on days 1-5, 14 and 21. The patient responded well to therapy, and his clinical symptoms improved. In follow-up after 28 days, his haematological parameters also improve.
Case study 2
A 30-year-old male presented with complaints of fatigue, dry cough, low-grade fever and progressive shortness of breath for the last two weeks. He was homosexual and had two male partners in the last year. He was diagnosed HIV Positive 2 years back and was on HAART. He was provisionally diagnosed with community-acquired pneumonia and treated at his local hospital however, his condition did not improve. On examination, he had a temperature of 100oF, BP of 110/75 mmHg, HR of 130/minute, RR of 30/minute, and SPO2 of 88% on room air. On auscultation, he had bilateral basal crackles in the lungs. The rest of the physical exam, including the cardiovascular system and abdomen, was normal.
Diagnosis
Laboratory findings were within normal range, except for LDH levels of 257 IU/L and CRP was elevated to 16.8 mg/dL. His CD4+ cell count was 75 cells/mm3. Chest radiography revealed infiltrative shadows in the bilateral upper lung field. Chest high-resolution computed tomography (CT) revealed a ground-glass opacity with multiple cysts on the bilateral upper lobes. Bronchoscopy was performed, and bronchoalveolar lavage revealed PCP by direct immunofluorescent assay.
Treatment
Oral TMP-SMZ and fluconazole were started on the first day of treatment. His respiratory condition improved on day 9 and was discharged. On follow-up after three weeks, he was doing well without recurrence of respiratory problems.
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Rudra Sahu is a practising physician and diabetologist from Raipur, Chhattisgarh.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries