How to Prevent Chronic Kidney Disease Progression
M3 India Newsdesk Jan 10, 2024
The article provides a comprehensive overview of CKD. It emphasises multifactorial causes and comprehensive treatment strategies along with targeted medications, and disease-specific interventions to manage and mitigate its progression.
Chronic kidney disease (CKD) is defined as a progressive and irreversible loss of renal function evidenced by an estimated glomerular filtration rate (eGFR) of <60 mL/min per 1.73m2 lasting for more than 3 months. The prevalence of CKD is rapidly increasing owing to an increase in diabetes mellitus, hypertension, and obesity.
Factors which increase risks of CKD progression
- Male gender
- Lifestyle factors
- High salt intake
- Smoking
- Obesity
- Systemic factors
- Diabetes mellitus
- Hypertension
- Connective tissue disorders
- Systemic sepsis
- Renal factors
- Low GFR
- Proteinuria
- Tubulointerstitial nephritis
- Obstructive uropathy
- Nephrotoxic drugs and agents like i.v. contrast
- Genetic factors
- Anaemia
- Metabolic acidosis
Avoidance of AKI in CKD
AKI is associated with significant morbidity and mortality, including an increase in adverse renal outcomes. AKI superimposed on patients with pre-existing CKD can cause further renal deterioration to end-stage kidney disease. The risk factors associated with AKI include older age, delayed renal function recovery from AKI, severe AKI episodes, the presence of proteinuria, and comorbidities such as DM, hypertension, and heart failure.
The treatment for Aki depends on the underlying etiologies and includes the optimisation of volume and hemodynamic status, the withdrawal of nephrotoxic agents, the adjustment of medication doses according to renal function and maintaining higher mean arterial pressure in patients with underlying hypertension. Drug regimens should be reviewed carefully to prevent drug-drug interactions.
Aetiology-based treatment strategy for CKD
1. Glomerulopathy
The major risk factors for a faster GFR reduction include significant proteinuria and CKD at the diagnosis of pathologically chronic renal lesions (glomerulosclerosis, tubular atrophy, and interstitial fibrosis).
Treatment depends on underlying etiology which includes:
- Dietary salt restriction
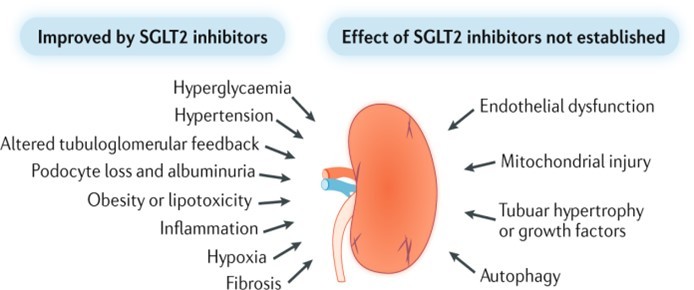
- SGLT2 inhibitors
- RAAS blockades
- Blood pressure control
- Diuretics
- Lipid-lowering agents
- Anticoagulation (prevent or treat thromboembolism)
- Immunosuppressive therapy: Steriods, calcineurin inhibitors, mycophenolate, rituximab
2. Diabetes mellitus-related CKD
- Adequate glycemic control
- RAAS blockade benefits
- Reducing glomerular capillary pressure.
- Decreases tubulointerstitial fibrosis.
- Decrease Major adverse cardiovascular events.
- Sglt2 inhibitors
- Other drugs: Finerenone, pentoxifylline, fenofibrate and GLP-1 analogues
3. Hypertension-related CKD
BP lowering is one of the most important management strategies for hypertensive patients with CKD. Target systolic BP<130 mmHg in patients with CKD and proteinuria would be reasonable.
In proteinuric CKD patients, intensive BP control is associated with a lower occurrence of serum creatinine doubling or ESRD.
Of note, Kidney Disease Improving Global Outcomes (KDIGO) updated the treatment target of SBP control to <120 mmHg in patients with hypertensive CKD.
Treatment includes:
- Salt restriction
- Smoking cessation
- Weight loss and adequate exercise
- Pharmacotherapy :
- RAAS blockades.
- Carvedilol.
- Mineralocorticoid receptor antagonists (MRAs), such as spironolactone, can reduce proteinuria and BP but are limited in the treatment of CKD due to their association with GFR decline and hyperkalemia.
- Novel nonsteroidal MRA: Finerenone.
Finerenone blocks MR-mediated sodium reabsorption and MR over-activation in both epithelial (e.g., kidney) and nonepithelial (e.g., heart, and blood vessels) tissues. MR over-activation is thought to contribute to fibrosis and inflammation
The nonsteroidal MRA Finerenone could improve renal and cardiac outcomes further in diabetics with kidney disease when added to renin-angiotensin system inhibitors
In patients with CKD and type 2 diabetes, treatment with Finerenone resulted in lower risks of CKD progression and cardiovascular events than placebo
4. Heart Failure-related CKD
- In addition to traditional medications to control HF, sacubitril, an angiotensin receptor–neprilysin inhibitor (ARNI), is currently recommended for patients with HF due to its significant benefits in reducing cardiovascular mortality and hospitalisation.
- Sacubitril/valsartan was recently found to help preserve renal function and reduce the severity of proteinuria in HF patients with a reduced ejection fraction.
5. Nephrolithiasis-related CKD
Nephrolithiasis significantly increases the risk of incident CKD and stone formers have a lower estimated GFR compared with those without renal stones. This phenomenon likely results from the fact that nephrolithiasis shares many risk factors with CKD, including:
- Nephrotoxic analgesic use for pain control during obstructive uropathy
- A decreased water intake leads to volume depletion
- An increased dietary protein intake
- Recurrent sepsis
- Urinary tract structural abnormalities
- Exposure to contrast media for imaging purposes
Notably, both operations and shock wave lithotomy induce renal parenchymal injury, inflammation, and fibrosis.
The prevention of stone formation may be a key step to improve outcomes. Patients with uric acid stones have also been found to have better renal outcomes when they receive xanthine oxidase inhibitors, especially febuxostat and maintain alkaline urine.
6. ADPKD associated CKD
V2 receptor antagonist tolvaptan in patients aged <55 years with an estimated GFR >25 mL/min/1.73 m2 can delay the worsening of kidney function and decrease the volume in a dose-dependent manner with adequate safety and tolerance.
Management of CKD complications
1. Metabolic acidosis
- The prevalence of metabolic acidosis was shown to increase linearly with GFR decline Metabolic acidosis can contribute to renal progression, and using alkali therapy was shown to slow renal progression.
- Metabolic acidosis is also associated with impaired bone mineralisation, insulin resistance, and higher all-cause mortality.
- Alkali therapy can be initiated early to achieve a serum HCO3− level between 22 and 26 mEq/L, since an HCO3− concentration >26 mEq/L is associated with higher mortality and cardiac events.
2. Anaemia
- Anaemia is a frequent complication of CKD and is associated with a poor prognosis. The correction of anaemia in CKD may enhance the quality of life for patients and reduce their renal function deterioration.
- Insufficient erythropoietin (EPO) production has been suggested as the major cause of renal anaemia and should be supplemented with erythropoietin injections.
- Recently, hypoxia-inducible factor (HIF) stabilisers, such as Desidustat have been developed for the treatment of renal anaemia. HIF, unlike ESAs, can bind to specific sequences called hypoxia response elements (HREs) to increase the production of endogenous EPO and to improve iron utility under hypoxia.
Diet and exercise
- A high protein intake causes hyperfiltration and increased intraglomerular pressure, resulting in the onset or progression of CKD.
- Therefore, dietary protein restriction has long been thought of as the mainstay of nutritional therapies for CKD. In general, dietary protein of 0.6–0.8 g/kg/day is suggested for stage 3 to 5 CKD patients without DM.
- Compared with animal proteins, plant proteins have less influence on glomerular hemodynamics and lower net acid production. A very low protein diet (0.3–0.4 g/kg/day protein) was reported to cause protein-energy wasting.
- Ketoanalogues are the precursors of essential amino acids, and their use with concomitant dietary protein restriction has been found to significantly delay the progression of CKD and to reduce the risks of dialysis initiation in patients with (estimated GFR >18 mL/min/1.73 m2) or without advanced CKD.
- Regular physical exercise is recommended for patients regardless of CKD stage and may benefit kidney outcomes.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries