How should a patient with chest pain be approached?
M3 India Newsdesk Apr 17, 2022
For clinicians, diagnosing a patient with chest pain can be tricky at times. This article, part of a new series on Clinical Decision Tools discusses how to handle patients with chest discomfort, emphasising rapid investigations, common and significant probable diagnosis, and treatment options.
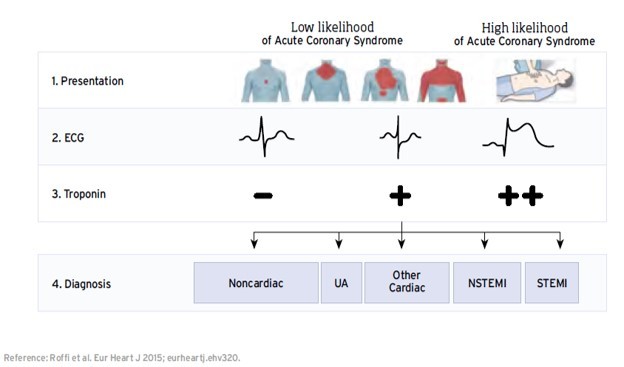
Initial assessment of patients with chest pain
Is this a life-threatening situation?
- Always begin with an ABCDE approach
- If the patient appears to be really ill or is on the verge of arrest, get assistance immediately
Concerning characteristics
- Over 120 beats per minute tachycardia, bradycardia, hypotension, rapid respiratory rate, and low GCS
- Sudden onset, excessive perspiration, nausea, vomiting, and pain radiating to the jaw, left arm, or back
- Alterations in the electrocardiogram
Consider the following
- Frequently occurring causes
- Cardiovascular system: myocardial infarction or acute coronary syndromes (STEMI, NSTEMI, unstable angina), and also pericarditis
- Respiratory system: Pneumothorax, pulmonary embolism, pneumonia
- Gastrointestinal tract: Reflux and peptic ulcer illness
- Musculoskeletal (others must be ruled out first)
-
Unusual but critical
- Dissection of the aorta
- Cardiac tamponade
- Sickle-cell crisis
History
- Presentation problem: Location and radiation, quality (heavy, hurting, sharp, tearing), severity (on a scale of 1–10), start and duration, accompanying symptoms (sweating, nausea, palpitations, breathlessness), aggravating or relieving variables (breathing, position, exercise, eating), recent trauma or effort, resemblance to prior episodes.
- Previous medical history: Cardiovascular or respiratory issues, diabetes, or oesophagal reflux
- Medication history: Heart or respiratory drugs, antacids, etc.
- Family history of coronary artery disease :(Especially in those under the age of 60), as well as premature cardiac death
- Social history: Smoking, tolerance for physical activity
Risk factors
- Ischaemic heart disease (IHD): Hypertension, elevated cholesterol, positive family history, smoking, diabetes, prior IHD, and obesity
- Pulmonary embolism: Prior PE/DVT, immobility, oestrogen/OCP usage, recent surgery, malignancy, family history, pregnancy, hypercoagulable conditions, smoking, and long-distance travel
- Gastrointestinal tract: Known GORD, known peptic ulcer, and alcohol excess
Monitor
Heart Rate, blood pressure (both arms), respiratory rate, saturation, and temperature
Examination
- General: pulse rate/rhythm/volume, excessive sweating, pallor, dyspnea, and cyanosis
- Neck: JVP elevated; trachea deviated
- Chest: Asymmetry in chest expansion/percussion/breathing sounds, discomfort in the chest wall, murmur
- Abdominal: Epigastric tenderness
- Legs: Swollen ankles, discomfort, oedema, and erythema in the calf
Investigative procedures
- ECG
- Blood- CBC, U&E, LFT, D-dimer (considering PE and low Wells score), troponin if suspected IHD
- ABG if patient is acutely unwell or saturation is <95%
- CXR
- Echo/CT if large proximal PE or aortic root dissection suspected- Additionally, echo can be used to detect regional wall motion abnormalities in MI
Reasons of chest discomfort that are frequent
| Diagnosis | History |
| Stable Angina | Exertional pain, radiating to left arm/jaw, <20 minutes, breathlessness, relieved by rest/GTN |
| ACS (Unstable angina) | Anginal pain at rest or with raised frequency, severity or duration |
| ACS (NSTEMI) | Sudden onset pain, radiating to left arm/jaw, >20 minutes, breathlessness, sweating, nausea |
| ACS (STEMI) | Sudden onset pain, radiating to left arm/jaw, >20 minutes, breathlessness, sweating, nausea |
| Pulmonary embolism | Breathlessness, PE risk factors, may have pleuritic chest pain and haemoptysis |
| Pericarditis | May have a history of viral-like illness, pleuritic pain, increased on lying, decreased by sitting forwards |
| Aortic dissection | Sudden onset severe interscapular pain, tearing in nature, breathlessness; may have arm weakness/numbness |
| Diagnosis | Findings examination |
| Stable Angina | Shortness of breath, tachycardia may be normal after pain resolves |
| ACS (Unstable angina) | Shortness of breath, ±arrhythmia, sweating |
| ACS (NSTEMI) | Shortness of breath, ±arrhythmia, sweating |
| ACS (STEMI) | Shortness of breath, ±arrhythmia, sweating |
| Pulmonary embolism | Often normal, may have evidence of DVT (swollen red leg), tachycardia, shortness of breath |
| Pericarditis | May have a pericardial rub, otherwise normal examinations |
| Aortic dissection | Tachycardia, shock, the difference in brachial pulses and pressures; limb weakness or paraesthesia |
| Diagnosis | Results on Investigations |
| Stable Angina | Transient ECG changes, troponin not elevated, positive stress ECG, positive coronary angiography |
| ACS (Unstable angina) | ST depression, T-wave inversion, troponin not elevated |
| ACS (NSTEMI) | ST depression, T-wave inversion; elevated troponin |
| ACS (STEMI) | ST-elevation or new LBBB, high troponin. |
| Pulmonary embolism | ABG: low (or normal) pO2, low CO2 (hyperventilation), clear CXR. Raised D-dimer. ECG: sinus tachycardia, S1Q3T3 (rare), thrombus on echo |
| Pericarditis | Saddle-shaped ST segments on most ECG leads, raised CRP |
| Aortic dissection | Widened mediastinum on CXR, aortic dilatation on echo/CT |
Management
- Oxygen saturation to be kept >94%.
- IV opioids can be considered (and an antiemetic) if the pain is more.
- Further treatment depends on the cause.
Diagnoses that are often made and critical
If a diagnosis cannot be confirmed quickly, consider life-threatening reasons and explore until they are ruled out.
- Cardiac ischaemia: Abnormal ECG, typical history, raised cardiac markers.
- Pulmonary embolism: Low sats, abnormal ECG, clinical risk, high D-dimer, positive CTPA.
- Pneumothorax: Mediastinal shift, decreased breath sounds, CXR.
- Aortic dissection: Evidence of shock, left and right systolic BP differ by >15 mmHg, mediastinal widening on CXR, abnormal CT/echo.
First medical contact in patients with chest pain (home ambulance)
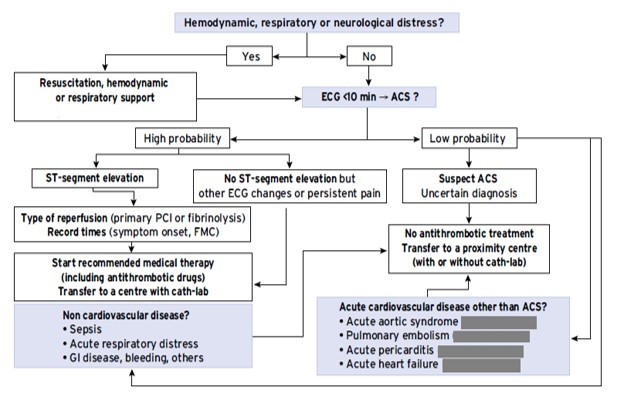
Management of patients with chest pain (emergency room)

Click here to see references
This article was originally published on 21 July, 2021.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries