High Altitude and Respiratory Complications
M3 India Newsdesk Apr 26, 2024
High altitude presents a unique and challenging environment for the human body and hence a prior knowledge of comorbidities and preventive modalities can go a long way in preventing morbidity and mortality besides the availability of emergency equipment and drugs.
More individuals are visiting high altitudes (>2000 m) due to the increased interest in adventure tourism, where the defining environmental feature is hypobaric hypoxia which sets in motion a series of important physiological responses that allow individuals to adapt to and tolerate the hypoxic conditions. In some cases, maladaptive responses predispose affected individuals to various forms of acute and chronic high-altitude illness.
Environmental factors at high altitude
Barometric pressure decreases in a nonlinear manner with increasing elevation and the inspired partial pressure oxygen (PiO2) falls, leading in turn to decreased alveolar and arterial oxygen tensions (PAO2 and PaO2, respectively). With increasing altitude, air density, humidity and temperature also decrease. This results in changes in pulmonary hemodynamics, insensible water losses, ventilatory shifts, and airway responsiveness.
Changes in pulmonary physiology at high altitude
Upon ascent to high altitude, the low PaO2 increases minute ventilation, known as the hypoxic ventilatory response (HVR). The HVR, which is mediated by the carotid bodies and raises PAO2 and PaO2, differs in strength in each person. HVR also causes a decrease in the arterial partial pressure of carbon dioxide (PaCO2); the resulting respiratory alkalosis leads to a leftward shift of the oxyhemoglobin dissociation curve, which improves alveolar oxygen uptake and – to a lesser degree – impairs oxygen delivery to the tissues.
Overall, the in vivo P50 stays roughly the same as that at sea level because of the leftward movement that is counterbalanced by the increased generation of 2,3-diphosphoglycerate by red blood cells upon ascent to high altitude. This mechanism also causes a compensating rightward shift in the curve.
Hypoxic pulmonary vasoconstriction (HPV) is another important physiologic response to acute hypoxic exposure which increases pulmonary vascular resistance and pulmonary artery pressure (PAP).
Respiratory disorders associated with acute exposure to high altitude
High-altitude pulmonary oedema
- The most important respiratory disorder associated with acute (hours to days) high-altitude exposure is high-altitude pulmonary oedema (HAPE) which is a noncardiogenic pulmonary oedema that may occur in unacclimatised people within 2-4 days of ascent to altitudes above 2500 m.
- In its early stages, it is characterised by increasing exercise intolerance and a dry cough, while in advanced cases individuals develop dyspnea at rest, cyanosis and a cough productive of pink, frothy sputum.
- Clinical findings include tachycardia, tachypnea, low-grade fever, hypoxemia, and unilateral or bilateral inspiratory crackles.
- When available, chest radiography shows patchy bilateral alveolar opacities; nevertheless, localised abnormalities, primarily in the right middle lobe, are possible in early HAPE.
- A previous history of the condition, male gender, quick ascent, greater altitudes, a history of respiratory infections, and intensive exercise are risk factors for HAPE.

Chest Radiograph in HAPE
- Slow rising to tall heights remains the best strategy to avoid HAPE. Over 3000 m people should not increment their resting rise by more than 300-500 m per night and should incorporate a rest day every 3-4 days to encourage acclimatisation.
- Nifedipine has been the backbone of avoidance for a long time, but later proved proposed that the phosphodiesterase-5 (PDE-5) inhibitor tadalafil and Sildenafil may moreover play a part in this respect. Information too bolsters a potential part for breathed in salmeterol.
- Acetazolamide and dexamethasone may moreover demonstrate to be advantageous in the anticipation of HAPE.
- Individuals who create HAPE close to a promptly available restorative office may be treated with supplemental oxygen and perception at the same elevation. When HAPE happens in more inaccessible areas absent from restorative care, as is frequently the case, a quick plummet is demonstrated and more often than not leads to the determination of the issue.
- Oxygen ought to be managed, or the person may be put in a versatile hyperbaric chamber to reenact a plummet to a lower rise.
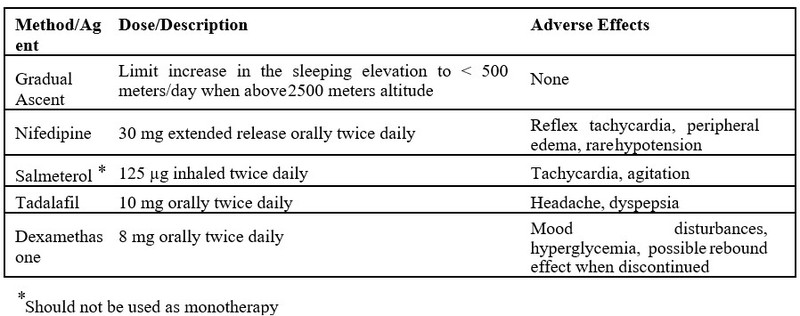 Pharmacologic and Non-Pharmacologic Measures to Prevent HAPE
Pharmacologic and Non-Pharmacologic Measures to Prevent HAPE
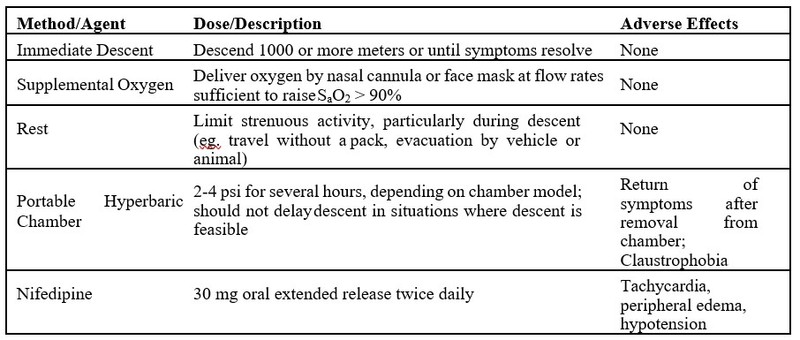 Strategies Used in the Treatment of HAPE
Strategies Used in the Treatment of HAPE
Acute Mountain Sickness (AMS)
AMS affects between 25 and 50% of unacclimatised low-landers ascending to altitudes between 2000 and 4200 m. Characterised by the presence of headache with malaise/fatigue, insomnia, dizziness or gastrointestinal symptoms (nausea, vomiting or anorexia).
People may be more susceptible to developing AMS if they have arterial hypoxemia in the first few hours of exposure to a hypoxic environment, whether it be simulated or real high altitude. Acetazolamide improves symptoms, decreases hypoxemia and prevents the progression of pulmonary dysfunction.
Periodic breathing
Periodic breathing (Cheyne-Stokes) occurs frequently in visitors to altitudes above 2000 m, and is almost universal after rapid ascent to elevations above 4000 m, even in the absence of acute altitude illnesses such as AMS or HAPE. It is marked by a crescendo-decrescendo pattern in tidal volume, punctuated by periods of apnea that can last anywhere from 5 to 20s. People often report restless sleep, racing thoughts and frequent nocturnal arousals, often with a distinct feeling of suffocation.
Theophylline and acetazolamide both decrease the frequency of periodic breathing. It has also been demonstrated that adding oxygen to the sleeping area increases the proportion of time in deep sleep stages, enhances subjective sleep quality, and lowers AMS scores the following day.
Respiratory disorders associated with chronic exposure to high altitude
As a result of maladaptive responses to chronic (months to years) hypobaric hypoxia, up to 5-10% of high-altitude residents in certain areas of the world develop one out of two forms of chronic high-altitude illness – chronic mountain sickness (CMS) and high-altitude pulmonary hypertension (HAPH).
Chronic mountain sickness (CMS)
- It occurs in persons who spend a year or more living at an elevation higher than 2500 metres.
- Polycythemia (haemoglobin >19 g/dl in females or >21 g/dl in males), persistent hypoxemia, and neurologic symptoms such as migraine headaches, lethargy, irritability, decreased attention, and acral paresthesias are characteristics of this illness.
- Moving to a lower altitude, doing phlebotomies regularly, isovolemic hemodilution, or taking extra oxygen are some forms of treatment. The long-term use of respiratory stimulants, such as medroxyprogesterone or acetazolamide, also improves oxygenation and polycythemia in CMS patients.
- Angiotensin-converting enzyme inhibitors such as enalapril may also be useful.
High-altitude pulmonary hypertension (HAPH)
HAPH is characterised by right ventricular (RV) enlargement and PH in the absence of polycythemia or neurologic dysfunction. HAPH is generally seen in long-term residents of altitudes above 2500 m but has been described in Indian soldiers posted to high elevations for periods of weeks to months. Affected individuals typically develop dyspnea, cyanosis, peripheral oedema, hepatomegaly and exercise intolerance.
The symptoms disappear with descent to lower altitudes. Nifedipine has been shown to decrease PAP in high-altitude residents. Tadalafil and sildenafil, two PDE-5 inhibitors, may also lessen PH caused by altitude.
Chronic lung disease at high altitude
A significant number of individuals with underlying lung diseases, such as asthma, chronic obstructive pulmonary disease (COPD), and pulmonary vascular abnormalities, are probably among the large number of people who go to high altitudes for business or pleasure.
Pulmonary vascular disorders
1. Pulmonary hypertension (PH)
Patients with PH may face an increased risk of HAPE with ascent to high altitude. Patients with PH may also be at risk for other complications, including worsening RV function, ischemia and worsening hypoxemia. Any additional rise in PAP brought on by HPV after ascent may decrease function or dilate the RV, which would reduce subendocardial blood flow and cause ischemia and chest discomfort.
2. Thromboembolic disease
- While several case reports describe venous thromboembolism occurring at high altitudes, systematic investigations have not found a higher incidence of venous thromboembolic events (VTEs) in this setting.
- While exposure to high altitudes may not affect everyone's chance of developing VTEs, it may have an impact on people who already have a coagulation issue.
- Individuals who are currently on an anticoagulant regimen ought to continue taking these drugs during their stay.
- Before going to a high altitude, patients with a history of VTE or hypercoagulable disease might want to think about stopping their oral contraceptives.
- All patients should be advised to avoid dehydration, venous occlusion and prolonged immobility, as these factors may elevate the risk for VTE.
3. COPD
- Exposure to hypobaric hypoxia at high altitudes may alter physiological factors, possibly exacerbating the baseline disease state.
- In a hypobaric hypoxic setting, hypoxemia deteriorates in patients with COPD.
- There is a theoretical worry that bullae in COPD patients with bullous emphysema may enlarge and/or burst when exposed to decreasing air pressure.
- Secondary PH may predispose to HAPE or worsening RV function during high-altitude travel, as discussed previously.
- Long-term inhabitants of high altitudes with COPD are more likely to develop cor pulmonale, according to multiple studies.
- Over 3050 metres (10,000 feet) in height is not recommended for travel. During their high-altitude stay, people who are currently receiving supplemental oxygen should keep using it, but they should increase their flow rate both at rest and when they are exerting themselves.
- To find out if they require extra oxygen at high altitudes, patients with an FEV1 of less than 1.5L who are not receiving it should have a pretravel evaluation.
4. Asthma
Prolonged stays at high altitudes result in better symptom control for asthmatic patients. Higher altitude has been correlated with a lower incidence of exacerbations and nocturnal symptoms, as well as a lower incidence of asthma in children. In certain instances, this phenomenon has been linked to the lower allergen burden at higher altitudes. This is because the quantity of dust mites, which are allergens inversely correlated with quality of life and FEV1 in asthmatic patients, is lower at high altitudes. This change is linked to a decrease in T-cell and eosinophil activation.
5. Chest wall abnormalities
Pneumonia factors that increase the risk of issues at high altitudes include central sleep apnea, alveolar hypoventilation, PH, cor pulmonale, and right-to-left shunt. Kyphoscoliosis and other abnormalities of the chest wall that result in a restrictive ventilator pattern may be linked to these complications. Patients with moderate to severe kyphoscoliosis should have pulmonary function tests and potentially an echocardiogram before travelling at high altitudes to rule out PH.
Case study
The case
A 54-year-old male from Kolkata (near sea level), West Bengal plans a trip with his family to Gulmarg in Kashmir (a high-altitude, low-temperature zone). The family catches a flight to Srinagar airport and upon landing directly books a cab to Gulmarg. Everyone has a fun time till the next day when the subject starts with heaviness in his chest, shortness of breath and headache. He can barely walk and is rushed to the nearest hospital where his Spo2 is 86% on arrival and chest auscultation reveals wheezing and rales at bases.
Diagnosis and management
A chest X-ray displays signs of bilateral congested lungs. He is immediately shifted to a Srinagar hospital which is at a much lower location where he receives oxygen inhalation and a Chest CT scan is done followed by 2 days in hospital treatment. He made a full recovery and was discharged with a diagnosis of High Altitude Pulmonary Edema and given specific advice to prevent it in future.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Waseem Ud Din is a practising pulmonologist from Srinagar.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries