Diabetes Related Foot Infections: IDSA Latest Updates
M3 India Newsdesk Feb 01, 2024
This article delves into the most recent guidelines issued by IDSA for the management of diabetic foot infections (DFI), offering insights into recommendations. It emphasises the prescribed antibiotic courses and cautions against certain treatments lacking evidence-based support.
The prevalence of diabetes is increasing with every passing day. The rising number of cases results in the rise of foot complications, including infections along with other complications associated with diabetes.
Diabetic foot infections (DFI) are associated with substantial morbidity resulting in high healthcare costs. DFI remains the most frequent complication associated with diabetic foot requiring hospitalisation and the most common precipitating factor resulting in amputation of the affected extremity.
List of recommendations
1. Diagnose a soft tissue diabetes
- Related infection is clinically based on the presence of local or systemic signs and symptoms of inflammation.
- The severity of any Diabetes-related foot infection (DFI) should be assessed using the International Working Group on the Diabetic Foot (IWGDF)/Infectious Diseases Society of America (IDSA) classification scheme (Table 1)

2. As per recommendation, hospitalisation should be considered in all persons with diabetes and a foot infection who have either a severe foot infection as per classification or a moderate infection which is associated with key relevant morbidities.
3. Inflammatory serum biomarkers such as:
- C-reactive protein (CRP), erythrocyte sedimentation rate
- (ESR), or procalcitonin (PCT) should be assessed in a person with diabetes and a possible infected foot ulcer for whom the clinical examination is diagnostically equivocal or uninterpretable.
4. As per recommendation consider a sample for culture to determine the causative microorganisms, preferably by aseptically collecting a tissue specimen (by curettage or biopsy) from the wound in a patient with DFI.
5. In a person with diabetes, consider using a combination of probe-to-bone tests, plain X-rays, and ESR, CRP, or PCT as the initial studies to diagnose osteomyelitis of the foot.
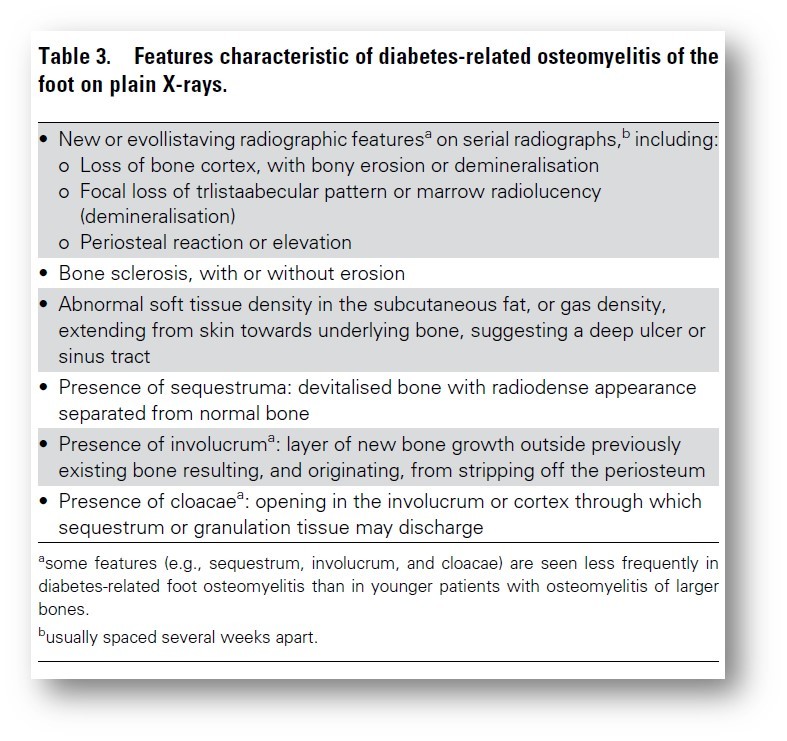
6. Magnetic resonance imaging (MRI) should only be ordered when the diagnosis of diabetes-related osteomyelitis of the foot remains in doubt despite clinical, plain X-rays and laboratory findings. PET, leucocyte scintigraphy or SPECT can be used as an alternative to MRI to diagnose osteomyelitis of the foot.
7. As per recommendation clinically uninfected foot ulcers should not be treated with systemic or local antibiotic therapy when the goal is to reduce the risk of new infection or to promote ulcer healing.
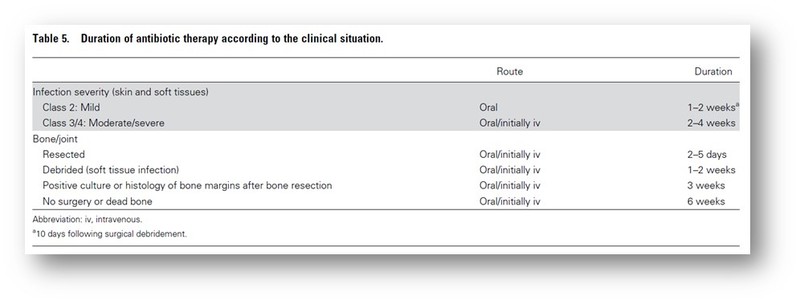
8. Course of antibiotics:
- Systemic antibiotics should be selected as per guidelines, the antibiotics should be administered for 1-2 weeks for skin or soft tissue DFI.
- If the wound is extensive and the patient has severe peripheral artery disease (PAD) consider continuing treatment for up to 3-4 weeks.
- Re-evaluation should be considered in patients not showing resolution of infection after 4 weeks of appropriate antibiotic therapy.
9. As per recommendation empirically target antibiotic therapy against Pseudomonas aeruginosa in cases of DFI in temperate climates should not be used, but the use of empirical treatment of P. aeruginosa is indicated if it has been isolated from cultures of the affected site within the previous few weeks, in a person with moderate or severe infection who resides in Asia or North Africa.
10. Cases with minor amputation for diabetes-related osteomyelitis of the foot should be considered for 3 weeks of antibiotic therapy and diabetes-related foot osteomyelitis without bone resection or amputation and positive bone margin culture consider antibiotic therapy for 6 weeks.
11. urgent surgical consultation should be obtained in cases of severe infection or moderate DFI complicated by extensive gangrene, necrotising infection, signs suggesting deep (below the fascia) abscess, compartment syndrome, or severe lower limb ischaemia.
12. Early (within 24–48 h) surgery combined with antibiotics should be considered for moderate and severe DFIs to remove the infected and necrotic tissue.
13. In people with diabetes, PAD and a foot ulcer or gangrene with the infection involving any portion of the foot obtain an urgent consultation by a surgical specialist as well as a vascular specialist to determine the indications and timings of a drainage and/or revascularisation procedure.
Surgical resection of infected bone combined with systemic antibiotics should be considered in a person with diabetes-related osteomyelitis of the foot.
14. Consider antibiotic treatment without surgery in cases of
- Forefoot osteomyelitis without an immediate need for incision and drainage to control infection,
- Without PAD
- Without exposed bone
15. As per recommendation the following treatments should not be used to address DFIs:
- Adjunctive granulocyte colony-stimulating factor (G-CSF) treatment.
- Topical antiseptics, silver preparations, honey, bacteriophage therapy, or negative pressure wound therapy (with or without instillation).
16. As per recommendation topical (sponge, cream, and cement) antibiotics in combination with systemic antibiotics should not be used for treating either soft-tissue infections or osteomyelitis of the foot in patients with diabetes.
17. As per recommendation Hyperbaric oxygen (HBO) therapy or topical oxygen therapy should not be used as an adjunctive treatment for the sole indication of treating a DFI.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries