Fluid Management in Critical Care
M3 India Newsdesk Sep 07, 2023
ICU patients often have conditions that impair their ability to regulate their hydration status. This article discusses the types of fluid administered in critical care along with the evaluation of the volume status and associated complications.
Fluid management in ICU
Improper fluid management leads to significant morbidity and mortality in ICU patients. Thoughtful consideration of the type and amount of fluid required for each patient is crucial. Fluids are by far the most commonly administered intravenous treatment in patient care.
During critical illness, fluids are widely administered to maintain or increase cardiac output, thereby relieving overt tissue hypoperfusion and hypoxia.
Evaluation of volume status
1. Physical examination
- Heart rate: Tachycardia can represent a compensatory physiologic response to maintain perfusion in the setting of hypovolemia.
- Blood pressure: Hypotension is suggestive of hypovolemia or sepsis.
- Respiratory rate: Increased respiratory rate indicates a compensatory response to metabolic acidosis from lactic acidosis due to poor tissue perfusion.
- Urine output: Expect a minimum of 1.5 mL/kg per hour in children and greater than 1 mL/kg per hour in adults
- Oedema: Peripheral oedema/ sacral oedema can be a sign of volume overload or third spacing of intravascular fluid.
- Peripheral pulses: Fast and thready pulses in dehydration states.
- Skin turgor and eyeball appearance: Severe cases of dehydration might present with flaccid or tented skin; Eyeballs might also appear sunken back into orbital cavities.
- Tactile temperature of skin: Classically find cool and clammy skin found in hypovolemic shock due to peripheral vasoconstriction causing hypoperfusion of skin, especially at the extremities.
- Mucous membranes: Dry, sandpaper-like texture of the oral mucosa or tongue in states of dehydration.
- Jugular vein appearance: Appreciate a distended jugular vein in a volume overload state; can also be found in patients with congestive heart failure.
Laboratory findings
- BUN/creatinine: Can be elevated secondary to prerenal acute kidney injury from decreased renal blood flow due to decreased intravascular volume.
- Transaminases: Can see an elevation in AST or ALT due to hypoperfusion of hepatic tissue and subsequent tissue hypoxia causing hepatocyte injury, also known as “shock liver.”
- Haemoconcentration: Can see elevated hematocrit due to a relative abundance of red blood cells relative to intravascular fluid volume.
Types of fluids
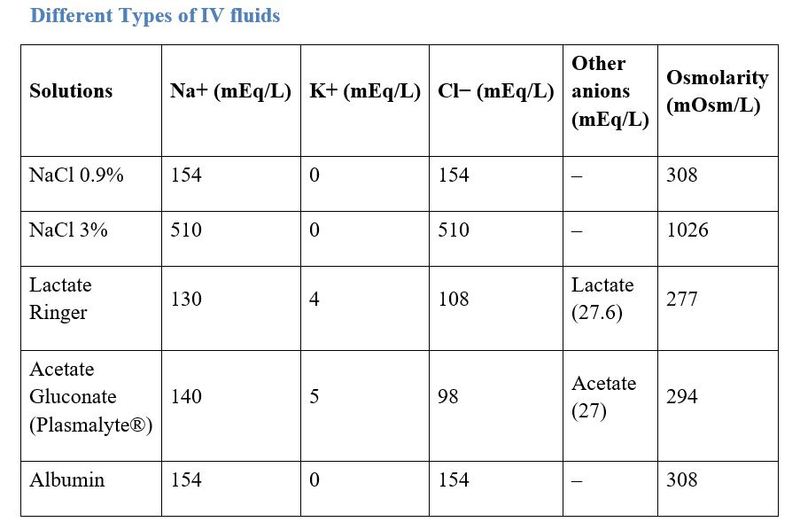
Crystalloids
Crystalloids have prudently been selected as the first choice for fluid resuscitation. Unbalanced crystalloid solutions (i.e. saline solutions) typically contain high concentrations of sodium chloride and have a pH that is lower than 6.0. The characteristics of saline solutions depend on their salt concentration (0.9, 0.45, 3% etc.). Balanced crystalloid solutions (e.g. Ringer’s lactate, Plasma-Lyte) are buffered by anions other than chloride. The concentration of chloride in 0.9% saline solution exceeds that of plasma (154 mEq/L).
Studies have shown that high renal tubular chloride concentrations induce renal afferent vasoconstriction with a resultant decrease in renal blood flow and GFR.
Administration of isotonic saline has been shown to cause hyperchloremic acidosis in both non-critically ill and critically ill patients. In healthy human volunteers, administration of intravenous 0.9% saline has also been shown to decrease renal blood flow velocity and renal cortical tissue perfusion when compared to a balanced solution (e.g. plasma-Lyte).
Given that the availability and cost of saline and balanced crystalloids are not significantly different, saline should probably no longer be used for intravascular volume expansion.
Colloids
Colloids contain macromolecules such as hydroxyethyl-starch (HES), gelatin, dextran, or albumin. It remains unclear whether albumin confers either benefits or risks in terms of mortality and renal function.
Given the cost of human albumin, it should generally not be considered the first choice for fluid replacement unless there is a specific indication for its use.
The evidence on gelatins remains clearly insufficient; few RCTs have been sufficiently powered to reveal valid patient-centred outcomes.
Fluid administration in specific conditions
1. Sepsis and septic shock
- The fluid challenge technique be applied where fluid administration is continued as long as hemodynamic factors continue to improve
- Crystalloids are the fluid of choice for initial resuscitation and subsequent intravascular volume replacement in patients with sepsis and septic shock.
- Lactic acidosis is a major metabolic side effect of sepsis. Intravenous administration of 0.9% saline may cause iatrogenic hyperchloremic acidosis. Reduced rates of mortality and AKI have been described with balanced solutions therefore until more information from RCTs is available, balanced solutions remain preferred over 0.9% saline for the treatment of hemodynamically unstable septic patients.
- Hydroxyethyl starch is not recommended for intravascular volume replacement in patients with sepsis or septic shock
- Albumin:
- If acute hypovolemia is not responsive to crystalloids alone, the use of human albumin can be considered.
- Albumin is the main determinant of plasma oncotic pressure and has a pivotal role in regulating fluid dynamics at the microvascular level.
- Albumin also performs other functions that may be relevant for septic patients.
- These include stabilisation of the glycocalyx, transport of molecules, antioxidant effects, immuno-modulation and positive inotropic effects.
2. Major bleeding and coagulopathy following trauma
- Fluid therapy using isotonic crystalloid solutions should be initiated in the hypotensive bleeding trauma. Excessive use of 0.9% NaCl solution is avoided.
- Hypotonic solutions such as Ringer’s lactate should be avoided in patients with severe head trauma.
- Colloids should be restricted due to the adverse effects on haemostasis.
3. AKI in perioperative period and in ICU
- Preferential use of crystalloid instead of colloid for fluid loading.
- Administering hydroxyethyl starch in the ICU increases the chances of RRT
- After hemodynamic stabilisation, avoid fluid overload.
4. ARDS
- Fluid restriction is advisable.
- After achieving hemodynamic stabilisation, fluid overloading may worsen ARDS.
Complications
1. Hyponatraemia
This is more of a risk when using hypotonic solutions. Many patients admitted to the hospital have risks of baseline elevated antidiuretic hormone (ADH) release leading to volume retention and worsening hyponatraemia. Isotonic fluids are preferred for maintenance fluids in patients with the syndrome of inappropriate antidiuretic hormone secretion (SIADH).
2. Hyperkalaemia
Patients with renal failure who receive a potassium-containing solution might not handle clearing the potassium load and develop life-threatening hyperkalaemia-causing cardiac arrhythmias.
3. Volume overload
Monitor for peripheral oedema, pulmonary oedema, or hepatomegaly. It is important to consider underlying cardiac dysfunction or renal failure and adjust volumes of administration accordingly. These patients might require a lower maintenance fluid rate than expected for their body weight.
4. Metabolic acidosis
Normal saline is a slightly acidic solution relative to normal body pH. This can precipitate metabolic acidosis. Lactated ringers solution is a closer approximation to normal body ph.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries