ESH 2023 Hypertension Guidelines
M3 India Newsdesk Jul 21, 2023
This article gives insight into the latest guidelines for hypertension released by the European Society of Hypertension in June 2023. These new guidelines will help the treating clinician manage hypertension effectively and to prevent hypertension-mediated organ damage.
The ESH 2023 hypertension guidelines closely resemble the 2018 ESH guidelines with incremental changes. The guidelines give emphasis on classification, clear guidance on the measurement of blood pressure especially on out-of-office blood pressure measurement, threshold for starting treatment, blood pressure targets, treatment and true resistant hypertension.
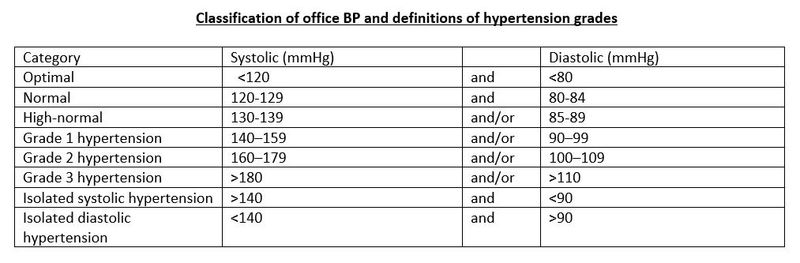
Definition and classification
The definition of hypertension remains unchanged from the previous guidelines ― repeated office systolic blood pressure values of ≥140 mm Hg and/or diastolic blood pressure values of ≥90 mm Hg.
As per recommendation blood pressure (BP) to be classified as optimal, normal, high normal, or grade 1, 2 or 3 hypertension, according to office BP.
 In addition to grades of hypertension, which are based on BP values, it is recommended to distinguish stage 1, 2, and 3 hypertension.
In addition to grades of hypertension, which are based on BP values, it is recommended to distinguish stage 1, 2, and 3 hypertension.
- Stage 1: Uncomplicated hypertension without HMOD, diabetes, CVD and without CKD ≥ stage 3. This stage is categorised as low to high risk.
- Stage 2: Presence of HMOD, diabetes, or CKD stage 3. This stage is categorised as moderate, high, and very high risk.
- Stage 3: Presence of CVD or CKD stage 4 or 5. This stage categorised is as a very high risk.
Risk assessment in hypertension with SCORE2 and SCORE2-OP
As per recommendation estimation of total CV risk is important in each hypertension patient because of its relevance in hypertension management. CV risk assessment with the SCORE2 and SCOR2-OP system is recommended for hypertensive patients who are not already at high or very high risk due to established CVD or CKD, long-lasting or complicated diabetes, severe HMOD (e.g. LVH) or a markedly elevated single risk factor (e.g. cholesterol, albuminuria).
Parameters for risk stratification which are included in SCORE2 andSCORE2-OP:
- Sex
- Age
- Level of SBP
- Smoking current of past history
- Non-HDL cholesterol
- Assessment of HTN-mediated organ damage (HMOD)
- Structural and functional changes in arteries and organs (brain, kidney, heart, eyes) caused by elevated BP
- Marker of preclinical/ asymptomatic CV/ kidney disease
- CV risk increase with the presence, extent and number of HMOD

Screening for hypertension and hypertension-mediated organ damage (HMOD)
- Case finding or opportunistic screening for hypertension is recommended in all adults.
- Regular BP measurements are recommended in adults from the age of 40 years or earlier in patients at high-risk.
- In individuals without hypertension, intervals for repeated BP measurement should be scheduled depending on the BP level, the risk of hypertension and CV risk. In patients with high risk, annual follow-up is recommended.
A basic screening test for HMOD is recommended for all HTN patients, the patients developing HMOD need to screen extensively to avoid further damage with proper intervention if required.
- 12 lead ECG
- Urine albumin creatinine ratio
- eGFr
Extended screening for HMOD
- Echocardiography
- Cf PWV (Carotid to femoral) or baPWV (brachial artery pulse wave velocity)
- Carotid artery ultrasound
- Coronary artier calcium score
- Abdominal aorta USG
- Kidney USG
- Ankle-brachial index (ABI)
- Retina microvasculature
- Brain imaging (CT, MRI)
Devices for BP measurement
Great emphasis has been given to the measurement of BP in these guidelines and clinicians should try to implement this in their practice to avoid error in diagnosing and managing hypertension.
- Automatic electronic, upper-arm cuff devices are recommended for office and out-of-office BP measurements (home and ambulatory).
- Hybrid manual auscultatory devices with LCD or LED display, digital countdown, or shock-resistant aneroid devices can be used for office BP measurement if automated devices are not available.
- Only properly validated devices should be used. Cuffless BP devices should not be used for the evaluation or management of hypertension in clinical practice.
Office BP measurements
-
Office BP is recommended for diagnosis of hypertension because it is the one method by which hypertension-related risk, benefits of antihypertensive treatment, and treatment-related BP thresholds and goals are based.
- Office BP measurements should be performed in standardised conditions, using a standard measurement protocol. Triplicate measurements should be taken and the average of the last two should be referred to as the representative value.
- It is recommended to diagnose hypertension during at least 2 separate office visits (within 4 weeks) unless office BP indicates grade 3 hypertension (≥180/110 mmHg) or patients present with hypertension-related symptoms or there is evidence of HMOD or CVD.
- At the first office visit, BP should be measured in both arms. A consistent between-arm SBP difference >15-20 mmHg suggests atheromatous disease and is associated with increased CV risk. All subsequent measurements should be made on the arm with the highest BP readings.

Home BP monitoring (HBPM)
- HBPM is recommended in addition to OBPM to improve CV risk due to better reproducibility and prognostic value than OBPM, although lacking data on treatment benefits from RCTs. HBPM is recommended to identify white-coat hypertension or masked hypertension.
- HBPM is recommended for long-term follow-up of treated hypertension because it improves BP control, especially when combined with education and counselling.
- HBPM should be performed using automated upper arm-cuff BP monitors validated according to an established protocol.
- Home BP should be monitored for 7 (not fewer than 3) days with duplicate morning (with 1 minute between them) and evening measurements before office visits. Average home BP should be calculated after discarding readings of the first day.
Ambulatory BP monitoring (ABPM)
- ABPM is recommended in addition to OBPM to improve CV risk prediction due to better reproducibility and prognostic value than OBPM, although lacking data on treatment benefits from RCTs.
- ABPM is recommended to identify white-coat hypertension, masked hypertension and nocturnal BP phenotypes. Repeated ABPM may be necessary because these phenotypes have limited reproducibility.
- ABPM should be used to diagnose true resistant hypertension.
- ABPM should be measured using upper arm-cuff automated BP monitors validated according to an established protocol.
- The recommended frequency of measurements is 20 minutes during the day and night to minimise the risk of missing day or night periods.
Lifestyle modification
This should be counselled to every patient by the treating clinician as it has been associated with a decrease in BP by 4-8mmHg, improvement in CV health and outcome, Bolster effect of medicine, and decrease in the number of drugs needed and the largest reduction is seen in those with highest BP.
- In adults with elevated BP who are overweight or obese, weight reduction is recommended to reduce BP and improve CV outcomes.
- Preferred dietary products include vegetables, fruits, beans, nuts, seeds, vegetable oils, and fish and poultry among meat products. Fatty meats, full-fat dairy, sugar, sweetened beverages, and sweets should be limited. Overall, healthy dietary patterns including more plant-based and less animal-based food is recommended.
- In adults with hypertension consuming a high sodium diet (most Europeans), salt substitutes replacing part of the NaCl with KCl are recommended to reduce BP and the risk for CVD.
- Dietary salt (NaCl) restriction is recommended for adults with elevated BP to reduce BP. Salt (NaCl) restriction to < 5 g (~2g sodium) per day is recommended.
- Increased potassium consumption, preferably via dietary modification, is recommended for adults with elevated BP, except for patients with advanced CKD.
- Daily physical activity and structured exercise are recommended for adults with elevated BP to reduce BP and improve cardiovascular risk profile. It is recommended to strive for at least 150-300 minutes of aerobic exercise a week of moderate intensity, or 75-150 minutes a week of aerobic exercise of vigorous-intensity or an equivalent combination. Sedentary time should also be reduced and supplemented with dynamic resistance exercise (2-3 times per week).
- Adult men and women with elevated BP or hypertension who currently consume alcohol (≥3 drinks/day) should be advised that a reduction of alcohol intake close to abstinence will lower their BP.
- Alcohol should not be recommended for CVD prevention, as previous studies linking moderate consumption to lower CV risk are likely confounded.
- It is recommended to avoid excessive (binge) drinking to reduce BP, and the risks, particularly for haemorrhagic stroke and premature death.
- Smoking cessation, supportive care and referral to smoking cessation programs are recommended for all smokers to avoid ambulatory BP increases, reduce the risk of masked hypertension, and improve CV health outcomes.
- Reduced stress via controlled breathing exercises, mindfulness-based exercise and meditation may be considered.
Treatment
- In patients 18 to 79 years, the recommended office threshold for initiation of drug treatment is 140 mmHg for SBP and/or 90 mmHg for DBP.
- In patients ≥80 years, the recommended office SBP threshold for initiation of drug treatment is 160 mmHg.
- However, in patients ≥80 years, a lower SBP threshold in the range of 140 – 160 mmHg may be considered.
- The office SBP and DBP thresholds for initiation of drug treatment in frail patients should be individualised.
- In adult patients with a history of CVD, predominantly CAD, drug treatment should be initiated in the high-normal BP range (SBP ≥130 or DBP ≥80 mmHg).
BP target
- Patients 18 to 64 years old: The goal is to lower office BP to <130/80mmHg.
- Patients 65 to 79 years old: The primary goal of treatment is to lower BP to <140/80mmHg. However, lowering BP to below 130/80mmHg can be considered if treatment is well tolerated.
- Patients 65 to 79 years old with ISH: The primary goal of treatment is to lower SBP in the 140 to 150 mmHg range. However, a reduction of office SBP in the 130 to 139 mmHg range may be considered if well tolerated, albeit cautiously if DBP is already below 70 mmHg.
- Patients ≥80 years old: Office BP should be lowered to a SBP in the 140 to 150 mmHg range and to a DBP < 80 mmHg.However, a reduction of office SBP between 130 to 139 mmHg may be considered if well tolerated, albeit cautiously if DBP is already below 70 mmHg.
General recommendations for antihypertensive drug treatment
- BP lowering should be prioritised over the selection of specific antihypertensive drug classes because treatment benefit largely originates from BP reduction.
- Five major drug classes including, ACEis, ARBs, BBs, CCBs, and Thiazide/Thiazide-like diuretics have effectively reduced BP and CV events in RCTs.
- The initiation of therapy with a two-drug combination is recommended for most hypertensive patients. Preferred combinations should comprise a RAS blocker (either an ACE inhibitor or an ARB) with a CCB or Thiazide/Thiazide-like diuretic. Other combinations of the five major drug classes can be used.
- Initiation with monotherapy can be considered in patients with:
- Grade 1 hypertension and low-risk if BP is only marginally elevated (less than 150 mmHg SBP and 95 mmHg DBP)
- high-normal BP and very high CV risk
- frailty and/or advanced age
- If BP is not controlled with the initial two-drug combination by using the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination, usually a RAS blocker + CCB + Thiazide/Thiazide-like diuretic.
- If BP is not controlled with a three-drug combination by using the maximum recommended and tolerated dose of the respective components, it is recommended to extend treatment according to the recommendations for resistant hypertension.
- The use of single-pill combinations (SPCs) should be preferred at any treatment step, i.e. during the initiation of therapy with a two-drug combination and at any other step of treatment.
- The combination of two RAS blockers is not recommended due to the increased risk of adverse events, in particular AKI.
- Patients who are not able to tolerate beta blockers or have contraindications, such patients can be given non-DHP CCB at any step instead of DHP-CCB.
- BBs should be used at the initiation of therapy or at any treatment step as GDMT, examples:
- Heart failure with reduced ejection fraction HFrEF
- Anti-ischemic therapy in chronic coronary syndromes
- Heart rate control in Atrial fibrillation
- BBs can be considered in the presence of several other conditions in which their use can be favourable BB should be used as guideline-directed medical therapy in respective indications or considered in several conditions such as in women with childbearing potential and planning pregnancy, HTN disorders in pregnancy, HTN with tachycardia, emergency and urgency conditions.


Effects associated with withdrawal of BP-lowering drugs
- CCBs: Risk of angina
- BBs: Risk of angina and other complications in CAD patients
- Centrally acting agents: Sympathetic over activity (nervousness, tachycardia, headache, agitation and nausea for 36–72 h after drug cessation)
- Diuretics: Fluid retention, edema, HF decompensation
Recommendation of antiplatelet therapy in hypertension
Low-dose aspirin is not recommended for primary prevention in patients with hypertension. It is recommended for secondary prevention in hypertensive patients. The use of a polypill containing low-dose aspirin can be considered in hypertensive patients for secondary prevention.
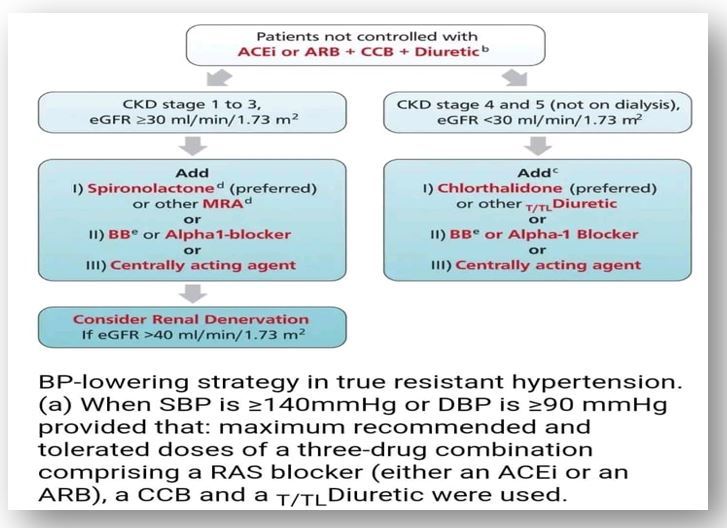
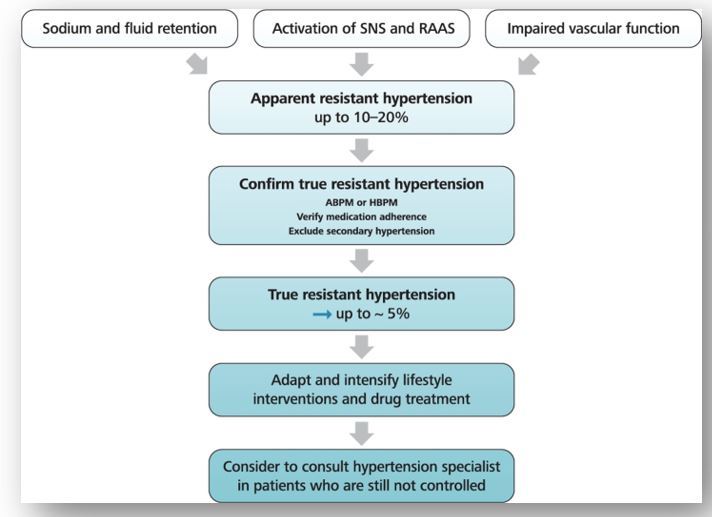
True-resistant hypertension
- It is recommended that hypertension is defined as true resistant hypertension when SBP is ≥ 140mmHg or DBP is ≥ 90 mmHg provided that:
- Maximum recommended and tolerated doses of a three-drug combination comprising a RAS blocker (either an ACEi or an ARB), a CCB and a Thiazide/Thiazide-like diuretic were used.
- Adequate BP control has been confirmed by ABPM.
- Various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
- It is recommended to manage resistant hypertension as a high-risk condition because it is frequently associated with HMOD and increased CV risk. The clinician should reinforce lifestyle measures.
- Drugs that can be considered as additional therapy in patients with resistant hypertension are preferably spironolactone (or other MRA), or BB or Alpha-1 blockers or centrally acting agents (clonidine), or amiloride (if available).
- Thiazide/Thiazide-like diuretics are recommended in resistant hypertension if estimated e GFR is ≥ 30 ml/min/1.73 m2.
- Loop diuretics may be considered in patients with an estimated eGFR < 45 ml/min/1.73 m2 and should be used if eGFR falls below 30 ml/min/1.73 m2.
- Chlorthalidone (12.5 to 25 mg once daily) could be used with or without a loop diuretic if eGFR is <30 ml/min/1.73 m2.
- Renal denervation can be considered as an additional treatment option in patients with resistant hypertension if eGFR is >40 ml/min/1.73m2.
White-coat hypertension (WCH) and masked hypertension
This is not so uncommon to have white coat hypertension in patients in clinical practice. One should not be in a hurry to label a patient as hypertensive and should follow the above mention recommendation for diagnosing HTN.
- Out-of-office BP measurement by ABPM and/or HBPM should be done when WCH is suspected, particularly in people with grade 1 hypertension.
- As per recommendation assessment of CV risk factors and HMOD should be done in patients with WCH.
- In patients with WCH, lifestyle interventions to reduce CV risk and close follow are recommended.
- Whether BP-lowering drug treatment should be used is still unresolved, but it can be considered in patients with HMOD and high CV risk.
Isolated systolic hypertension in the young (ISHY)
- Central BP measurement can be considered to identify ISHY individuals at low CV risk to detect spurious hypertension, if available.
- Close follow-up and lifestyle interventions are recommended. In individuals with high out-of-office BP or high central BP, particularly with other CV risk factors or HMOD, BP-lowering drug treatment can be considered.
Isolated diastolic hypertension (IDH)
As per recommendation, the BP-lowering drug treatment should follow the general treatment strategy.
Hypertension management during follow-up
- The first three months are important after initiation of treatment, the patient should visit (including virtual care visits) every month or more frequently if BP depends on hypertension grade. ABPM may be included in the follow-up examinations whenever possible.
- After the end of the titration phase, when BP is controlled less frequent visit is suggested. In cases unable to achieve BP control or having high CV risk frequent visits should be continued.
- The use of novel telehealth technologies and virtual care possibilities is recommended to improve hypertension management during follow-up. HBPM data should be shared with care providers with mobile phones, personal computers or internet links or cloud-based connectivity.
- As per recommendation HMOD should be also checked periodically. In patients without preexisting HMOD, subsequent checks can be done at longer intervals, e.g. every 3 years. Frequent checks should be performed in hypertensive patients with HMOD.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries