Emergencies in Diabetic Patients: Challenges and Management
M3 India Newsdesk Feb 21, 2024
This article provides a comprehensive overview of hypoglycemia and hyperglycemia. It emphasises the need for personalised care plans & collaboration with healthcare professionals to effectively manage diabetes and minimise the risk of acute and chronic complications.
Hypoglycemia
Hypoglycemia is commonly defined as a blood glucose level below 70 mg/dL. Some symptoms which patients experience are tremors, palpitations, diaphoresis, paresthesia, and hunger.
However, when the glucose level goes below the threshold of 54 mg/dL, patients may experience:
- A lack of concentration
- Headache
- Blurry vision
- Dizziness
- Confusion
- Seizures
- Speech disturbance
- Restlessness
- Loss of consciousness
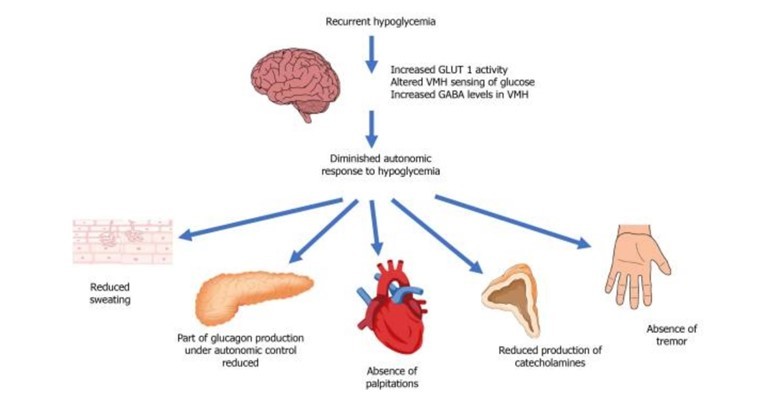
However, the threshold can drop further with recurrent episodes of hypoglycemia and rise in patients with uncontrolled diabetes.
Hypoglycemic unawareness occurs when patients have frequent hypoglycemic events which shifts glycemic thresholds for symptoms to lower plasma glucose concentrations, close to levels that cause cognitive failure.
Treatment protocol
In patients who are conscious, orientated, and able to swallow:
- Stop insulin (pump or IV infusion) immediately.
- Give 15-20 g rapid-acting carbohydrates of the patient’s choice where possible. Examples: chewable glucose tablets, orange juice, or 3-4 teaspoons of sugar dissolved in water (like Glucon-D).
- Measure capillary blood glucose 10-15 min later. If it is still less than 70 mg/dL, consider IV 200 mL of 10% glucose over 15 min or administration of 1 mg of glucagon IM.
- Once blood glucose is above 70 mg/dL and the patient has recovered, it is recommended to give a long-acting carbohydrate. Examples: a slice of bread, biscuits.
In patients who are conscious but confused, but able to swallow:
- Give a 15g tube of glucose if available, or glucagon 1mg IM.
- If capillary blood glucose 10-15 min later is still less than 70 mg/dL, give IV 200 mL of 10% glucose over 15 min.
- Once blood glucose is above 70 mg/dL, a long-acting carbohydrate can be given.
For patients who are unconscious and/or having seizures:
- Check - Airway, breathing, pulse, state of consciousness, blood glucose level, and temperature.
- Establish IV access and give 100 mL of 20% glucose IV or 200 mL of 10% glucose over 15 min.
- Blood glucose levels should be checked every 10 minutes to monitor improvement.
Hyperglycemia
Hyperglycemia is commonly defined as blood glucose than 125 mg/dL while fasting, and greater than 180 mg/dL two hours postprandial.
There are 2 main hyperglycemic emergencies:
- Diabetic Ketoacidosis – DKA is an acute, life-threatening emergency characterised by hyperglycemia and acidosis.
- Hyperosmolar hyperglycaemic states - HHS refers to severe persistent hyperglycemia, in the absence of ketosis, but accompanied by profound dehydration.
Treatment protocol:
These images provide an overview of how to treat DKA and HHS.
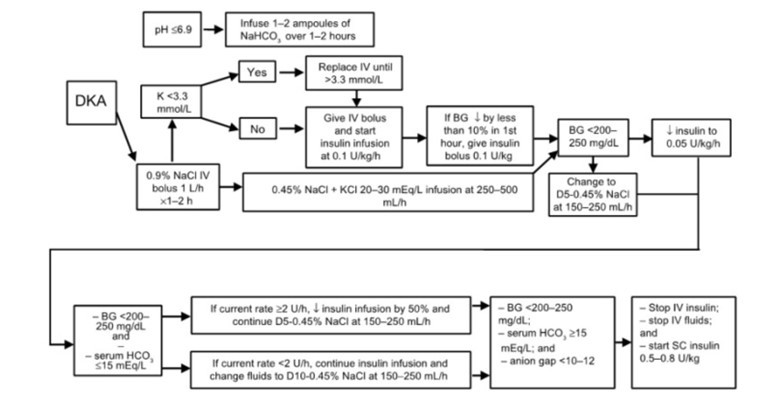
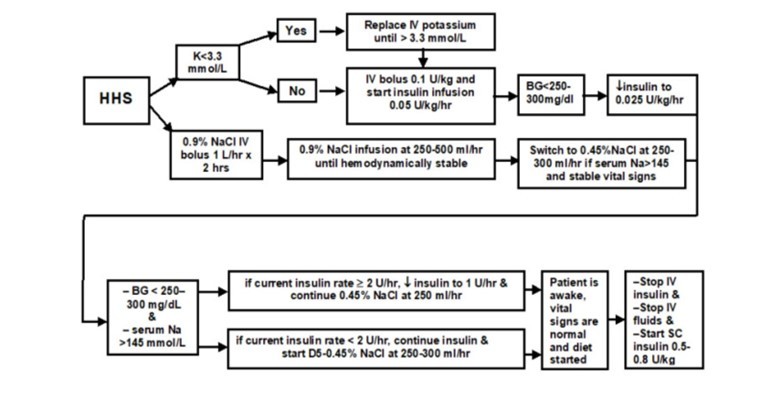
Fluid resuscitation
The IV fluid of choice in the management of DKA or HHS is Isotonic saline (0.9% Saline). Saline should be started at a rate of 10-20 ml/kg. At least 1 L of fluid should be administered within the first hour of presentation. Over the next 8 hours, 0.9% sodium chloride should be given in combination with potassium chloride to correct overall K+ depletion.
- 1 L over 2 hours
- 1 L over 2 hours
- 1 L over 4 hours
The patient should be re-evaluated regularly to assess the need for further fluid resuscitation or a change in the rate of infusion.
Insulin therapy
Insulin is administered by Fixed Rate IV Insulin Infusion (FRIII). The infusion dose is set based on the weight of the patient in kg. The dose is set at 0.1 units/kg/hour.
Before FRIII, a bolus dose + Variable Rate IV Insulin Infusion (aka VRIII/Sliding Scale) was the norm. However, there were some shortcomings to this. VRIII is disadvantageous as it is based on capillary blood sugar. Using a sliding scale allows for the control of blood sugars but does not facilitate the reduction of ketogenesis adequately.
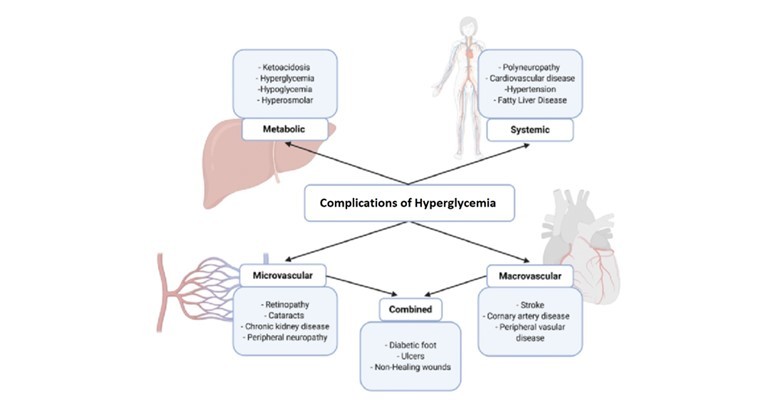
Complications
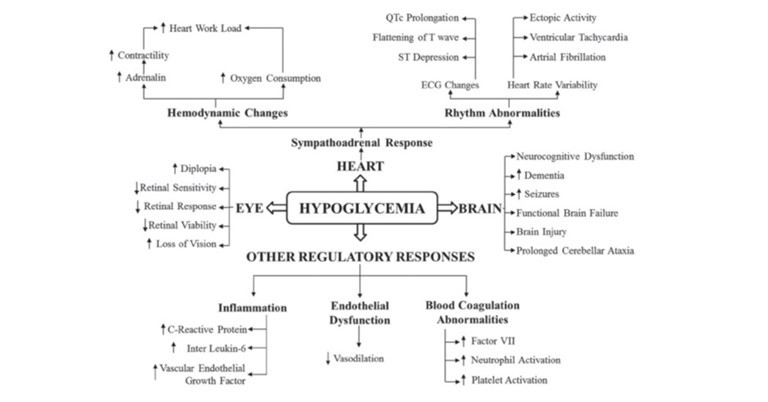
Both hypoglycemia and hyperglycemia, if not controlled or treated in time, can cause acute and chronic complications. The heart, brain and eyes are the most affected by diabetes.
Impact on quality of life
Patients with recurrent hypoglycemic or hyperglycemic episodes often feel powerless, irritable, and depressed. This also affects their near and dear ones.
- Travel: Driving over long distances needs concentration, hand-eye coordination and rapid decision-making. A hypoglycemic or hyperglycemic episode often affects those parameters, thereby increasing the risk of danger to self or others. Frequent flight travel among various time zones can increase the risk of diabetes becoming uncontrolled due to irregular meal times and unhealthy eating habits.
- Sleep: Cases of nocturnal hypoglycemia often go undetected. Patients may experience sleep disturbances, morning headaches, chronic fatigue, or mood changes.
- Employment: Frequent episodes of hypoglycemia or hyperglycemia at the workplace can be embarrassing or dangerous. It is especially dangerous for patients working underwater, in the mining industry, in oil rigs, or with heavy machinery.
Expert psychological counselling needs to be given to the patient and their family members. An individualised treatment plan can help decrease the frequency and severity of hypoglycemic or hyperglycemic episodes.
Medication adjustment
Choosing the appropriate drug and dose after a hypoglycemic or hyperglycemic event is important in managing treatment and preventing further episodes.
- Metformin, DPP-4 inhibitors, GLP-1 analogues, SGLT-2 inhibitors, and pioglitazone are associated with low risk of hypoglycemia in patients with type 2 diabetes.
- Sulfonylureas and glinides are associated with a higher risk of hypoglycemia.
- Both Metformin and Sulfonylureas help reduce HbA1c by around 1.5%. Renal function and weight gain should be monitored with Metformin. The dose of sulfonylureas should be adjusted to minimise the risk of hypoglycemia.
- Adjusting Insulin dose or adding short-acting Insulin can help reduce the blood glucose in a hyperglycemic event. Additionally, based on whether the fasting or postprandial glucose level is high, the medication doses must be adjusted accordingly.
- Early initiation of insulin therapy is advised if patients do not meet target glycemic goals.
- Medication changes are also warranted if the patient has recently lost weight from an exercise regime or gained weight due to less activity, based on the latest glucose levels.
- Hospitalisation is not required to start or adjust medications unless the diabetes is significantly uncontrolled and the patient is severely symptomatic or unable to hydrate adequately.
Prevention of hypoglycemia/hyperglycemia
- Make sure the patient and family members understand and agree to adhere to all aspects of the treatment plan. Awareness should be given about early identification of hypoglycemic symptoms, their causes, preventive measures, and available treatment options.
- Teach the patient the signs and symptoms of hyperglycemia and hypoglycemia and provide instructions on when to seek additional care.
- Regular measurement of blood glucose (even maintaining a journal) is the most effective way of capturing blood glucose trends and identifying asymptomatic hypoglycemia. Monitoring blood glucose before and after physical exercise can help prevent hypoglycemia. Small meals can be taken before a physical activity.
- The use of continuous glucose monitoring (CGM) in patients with uncontrolled diabetes (type 1 or type 2) contributed to improved glucose level control and reduction in HbA1c.
- Collaborate with a Nutritionist to make a personalised diet chart with a glycemic index of foods.
- Educate on the need for tightly controlled glucose levels of 80 to 120 mg/dl before meals and less than 180 mg/dl 2 hours after eating, and maintain the blood pressure to less than 130/80 mmHg.
- Stress the importance of annual eye, foot, and kidney function screenings to monitor vascular complications.
- Monitor HbA1c levels every 6 months.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Christus Gerald Herbert, Fellowship in Diabetology, AFIH, Lead Assistant Manager, SCIO Health Analytics, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries