Dry Eyes in Sjogren's Syndrome: Pathogenesis And Treatment
M3 India Newsdesk Sep 30, 2022
Primary Sjogren's syndrome ranks among the most common autoimmune diseases, with a prevalence rate ranging from 0.06% to 1.5%. The article describes the pathogenesis, assessment tools and treatment of dry eyes in Sjogren's syndrome.
Sjogren syndrome
Sjogren's syndrome is a chronic inflammatory autoimmune disease histopathologically characterised by lymphocytic infiltration of exocrine glands leading to a clinical picture of dry mouth(xerostomia) and dry eyes (keratoconjunctivitis sicca).
The prevalence of primary Sjogren’s syndrome is much higher in women than men (e.g., approximately 10:1), with a peak incidence in the fifth and sixth decades of life.
Pathogenesis
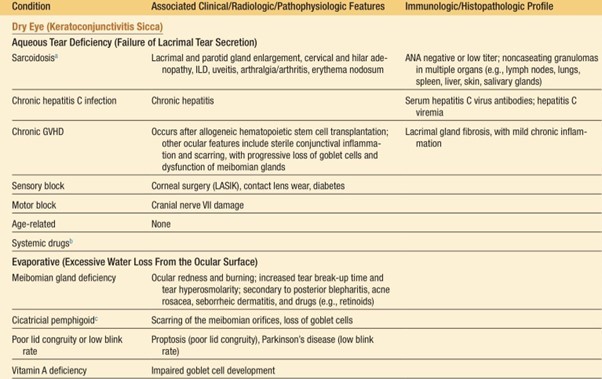
The anatomy of the tear film informs the differential diagnosis of a dry eye. The tear film consists of three major layers: the outer lipid layer, the middle aqueous layer, and the inner mucin layer. The middle aqueous layer is diminished in Sjogren’s syndrome. Conditions associated with infiltration of the lacrimal glands (e.g., sarcoidosis) and diminished tear flow (e.g., medications, ageing, and estrogen deficiency) may also decrease aqueous tear flow.
The lipid layer derives from the meibomian glands and traps the aqueous tear film on the eyeball and protects it from rapid evaporation. Meibomian gland dysfunction, or posterior blepharitis, produces dry eyes from rapid evaporation of tears; it often accompanies aqueous tear deficiency and can be an aggravating factor in patients with keratoconjunctivitis sicca that requires additional therapy.
Meibomian gland dysfunction is often associated with ocular rosacea and seborrheic dermatitis, two conditions that also lead to dry eyes. Lipid degradation resulting from meibomian gland inflammation leads to the production of free fatty acids, which irritate the ocular surface and in turn may cause punctate keratopathy.
The mucin layer originates from the goblet cells of the conjunctiva and, if deficient, leads to an uneven distribution of the tear film over the surface of the eye. Vitamin A deficiency and Stevens-Johnson syndrome are examples of conditions associated with an abnormal mucin layer.
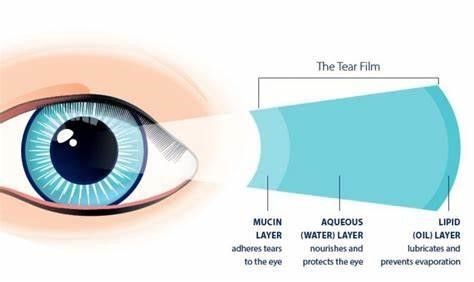
- Mucin layer: Vitamin A deficiency and Stevens-Johnson
- Aqueous layer: Sjogren’s syndrome
- Lipid layer: Posterior blepharitis
History
History of dry eyes may be elicited from the patient by the use of specific validated questions.
Ocular symptoms- The symptoms of dry eyes may be sought with questions such as:
- Have you had daily, persistent, troublesome dry eyes for more than three months?
- Do you have a recurrent sensation of sand or gravel in the eyes?
- Do you use tear substitutes more than three times a day?
Other causes of dry eyes
Eye manifestations:
Chronic inflammation of the lacrimal glands diminishes the secretion of aqueous tears, which, if severe, may destroy the conjunctival and bulbar epithelium. Aqueous tear deficiency produces a dry eye, causing symptoms of grittiness or foreign body sensation, burning, photophobia, and eye fatigue. Eye dryness, itching, and pain are often the first symptoms that lead to the investigation of possible Sjogren's syndrome
Vision-threatening diseases like uveitis, episcleritis/scleritis, optic neuropathy, retinal vasculitis, cicatrising conjunctivitis, sterile corneal ulcer/infiltration, or corneal melt/perforation are more frequent in primary Sjogren's syndrome.
Assessment tools
The ocular surface disease index is a frequently used questionnaire that consists of 12 questions probing dry eye symptoms. This distinguishes between normal subjects and those having dry eyes and can be used to measure the severity of the eye symptoms and their effect on visual function.
Eye examination
A routine eye examination usually reveals a reduction in the tear flow, as measured by the Schirmer-I test. Additional findings may include the absence of tears in the conjunctival sac and dilated bulbar conjunctival vessels. Thick mucus may also be seen in the inner canthus of the eye.
A)Tear film assessment method
Schirmer test is a standard assessment for measures of aqueous tear production (Fig. 4). Though it can be shortly troublesome for the patient, it is safe, easy to perform, and inexpensive and is demonstrated in the picture below. Although a Schirmer-I test has an approximately 20% false-negative rate, normal tear flow in the face of ocular foreign body sensations suggests an alternative diagnosis such as blepharitis.

B) Slit-lamp examination
It allows for a more detailed visualisation of the corneal and conjunctival surface. After the instillation of lissamine green dye or fluorescein onto the ocular surface, a slit-lamp examination may expose devitalised cells or epithelial defects, respectively, which are signs of corneal and conjunctival damage. A rapid tear break-up time (less than 10 seconds) can result from a deficiency of the aqueous or lipid layers of the tear film, and thus cannot distinguish between lacrimal gland destruction and blepharitis
C) Radiological investigations.
MRI and CT scans of the lacrimal gland are investigative techniques mostly used to differentiate between benign and malignant lesions, often when lacrimal glands present with unilateral swelling.
D) Other Laboratory Parameters
Special tests like Antinuclear antibody (ANA) should be done in patients suspicious of Sjogren’s syndrome. These patients tests positive for anti-Ro/SS-A and anti-La/SS-B antibodies, respectively, and approximately one-half of them test positive for Rheumatoid factor.
Treatment
First-line therapy is lubrication with tear substitutes, followed by anti-inflammatory eye drops. Preservative-free artificial tears are recommended to avoid local toxicity. Active ingredients of tear films include hydroxypropyl methylcellulose, carboxymethylcellulose, polyvinyl alcohol, hyaluronic acid, and liquid polyols. Low-viscosity tears are administered more often than high-viscosity tear formulations; the latter is most useful at bedtime for sustained lubrication during the sleeping hours
An ophthalmic preparation of cyclosporine, 0.05%, is used for the treatment of dry eyes related to Sjogren's syndrome. Lifitegrast is a novel ophthalmic preparation that reduces ocular inflammation. Tears may be conserved by blocking the nasolacrimal drainage channels with temporary or permanent occlusion, a relatively simple procedure performed by an ophthalmologist.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Radhika Jakhotia is a DNB resident in rheumatology from Manipal hospital.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries