Dialysis Day Care: An Overview
M3 India Newsdesk Feb 23, 2023
Dialysis is a form of renal replacement therapy, where the kidney's function of blood filtration is substituted by artificial equipment, which removes excess water, solutes, and toxins. The indications, duration and complications of dialysis are penned down in this article.
Dialysis
Dialysis ensures the maintenance of homeostasis in patients having loss of kidney function either acute kidney injury (AKI) or a prolonged, gradual loss that is chronic kidney disease (CKD).
There are two main types of dialysis
- Hemodialysis (HD)
- Peritoneal dialysis (PD)
The dynamics of this particular form of renal replacement therapy vary across countries with longer dialysis sessions and slower blood flow rates in Japan. PD is highly prevalent in Hong Kong and the Jalisco region of Mexico, while Home HD is widely adopted in New Zealand and Australia.
Indications for dialysis
- Acute kidney injury
- Uremic encephalopathy or pericarditis
- Refractory hyperkalemia
- Refractory Acidosis
- Hypervolemia with pulmonary oedema
- Asymptomatic patients with a GFR of <5 mL/min/1.73 m²
Equipment
Hemodialysis (HD) apparatus includes;
- Blood circuit
- Dialysis solution circuit
A dialyser bridges these circuits. Side ports attached to the bloodlines are used for saline or heparin infusion, air entry detection, and pressure measurements. The dialysate is pumped through the dialysate compartment, separated from the blood compartment by the dialyser's semi-permeable membrane.
Blood circuit
A roller pump moves blood through the dialyser. The pre-pump segment connects the vascular access to the blood pump and contains a saline infusion line, a sampling port, and a "pre-pump" pressure monitor. The heparin line delivers heparin at a constant rate throughout dialysis. A venous pressure alarm is attached to the venous line.
The dialysis fluid circuit includes;
- A water purification system.
- A proportionating system that mixes the water and concentrates and feeds it to the dialyser.
- Monitors, alarms, and ultrafiltration control with advanced control options.
Weight and fluid removal
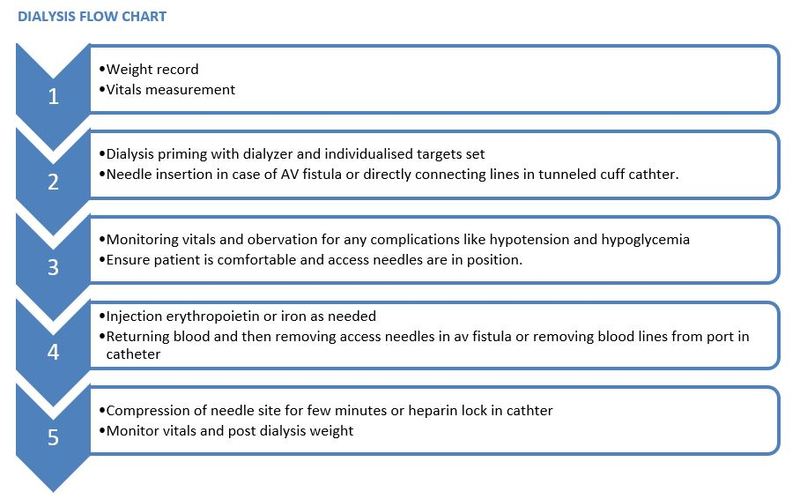
After a patient enters the dialysis daycare, weight is done on the standardised weighing machine. The weight is compared to the previous post-dialysis weight and his ‘dry weight’. Dry weight is your weight without any excess fluid and at which the blood pressure remains normal. The 'dry weight' probing approach helps evaluate dialysis adequacy and is associated with cardiovascular benefits.
Teamwork
A dialysis care team is an interprofessional group of qualified individuals contributing to holistic patient management and a smooth transition to a dialysis-dependent life. Nephrologists are team leaders with expertise in treating renal conditions. Advanced providers such as a nurse and dialysis technicians collaborate with nephrologists in managing kidney patients at the dialysis day care unit.
Medical officers are specialised in assessing dialysis patients, assuring proper administration of medications and treatment, and overseeing the dialysis process. They also supervise home programs training patients and their care partners in administering self-dialysis modalities like home hemodialysis and continuous ambulatory peritoneal dialysis (CAPD). The dietician helps plan meals and tailors the diet to meet each patient's unique needs.
The dialysis technician performs the dialysis treatment and monitors patients throughout, while biomedical technicians maintain the machines and water quality at the dialysis centre. The vascular access care team includes a vascular access surgeon who creates and maintains access to dialysis. The patient can sit and work on a laptop, eat food and watch television during the HD session. A record is maintained which includes the patient’s history, diagnosis, and weight record with inter-dialysis weight gain, blood reports and medications.
Preparation/Access for hemodialysis
The gold standard is the distal AV fistula. The alternatives are synthetic grafts and tunnelled central venous catheters.
Technique: A 15 or 16-gauge needle is inserted to access circulation. Blood is pumped through the dialyser at a rate of 300-500 ml/min while dialysate flows in a counter-current direction at 500-800 ml/min. Hemodialysis dose is individualised in every patient. The blood passes through the dialyser and then into the venous chamber and back to the patient. It is ensured the distance between the arterial and the venous needle on the patient’s side is maintained to avoid recirculation of dialysed blood back in the blood circuit.
Duration and frequency
The duration of dialysis is usually 4 hours but can be prolonged if excess fluid removal or clearance is targeted. The frequency of dialysis is at least two times per week but in case of low residual renal function, thrice-weekly hemodialysis might be required. Additional or more extended sessions are considered for patients with significant weight gains, poorly controlled blood pressure, high ultrafiltration rates, poor metabolic control, or difficulty achieving dry weight.
The chosen ultra-filtration rate for each session should allow for an optimal balance between achieving euvolemia, solute clearance, and adequate blood pressure control with minimal hemodynamic instability and intradialytic symptoms. Dialysis patients have a reduced health-related quality of life (HRQoL) associated with increased morbidity and mortality.
Complications
Intra-dialytic hypotension: It usually presents as dizziness, light-headedness, nausea, or subtle symptoms. Management includes giving Trendelenburg position and rapidly administering a 100 mL bolus of normal saline through the bloodline.
Muscle cramps: Hypotension, high ultrafiltration rate, Hypervolemia, and low-sodium dialysis solution predispose to cramps. When occurring concomitantly with hypotension, treatment with 0.9% saline is effective. Forced stretching of the muscle involved could provide relief.
Itching: It is a very common complaint usually due to dry skin and some unknown mechanisms. Treatment includes moisturising skin and antihistaminics. Some cases require difelikefalin.
Some reactions are medical emergencies requiring immediate stopping of dialysis, clamping of lines, and supportive care followed by definitive care. Examples of such complications are dialysis disequilibrium syndrome, hemolysis, air embolism and dialyser reactions.
Other nonspecific complications include nausea and vomiting, headache, and abdomen, chest and back pain.
Case studies
Case 1
A 70-year-old gentleman having diabetes, hypertension and chronic kidney disease is undergoing hemodialysis three times a week through left brachiocephalic A-V fistula for the past 1 year. He had complaints of muscle cramps and hypotension in the last 1 hour of hemodialysis.
Management
His complaints were of generalised weakness and fatigue after dialysis. Hence his dry weight was increased considering his actual lean body mass would have been increased. Following that with less ultrafiltration during each session he did not have any such symptoms.
Case 2
A 56-year-old female is suffering from diabetes mellitus, Ischemic heart disease with LV dysfunction and chronic kidney disease which needed initiation of hemodialysis for the past 2 months. She had complaints of persistent pedal oedema and dyspnoea on exertion which partially resolved after imitation of HD. But she had hypotension and arrhythmias after 2-3 hours of hemodialysis.
Management
Her dialysis sessions were increased to thrice twice per week. UF profiling and sodium profiling was done so that fluid removal was more in the beginning and dialysate sodium was gradually decreased during each session. Also, potassium was increased to 4meq in the dialysate compartment.
Future of dialysis
Wearable and implantable artificial kidneys are the future of hemodialysis, with lower operational costs helping overcome the infrastructural barriers to providing self-care treatment for renal failure. They employ a sorbent-based dialysis regenerative system called recirculating dialysate. An implantable artificial kidney employs silicon nanotechnology and tissue engineering to produce a surgically implanted device that mimics a native kidney.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries