Diabetic Retinopathy: Screening Recommendations, and Treatment Options
M3 India Newsdesk Apr 30, 2024
Unravel the mystery of diabetic retinopathy, a sight-threatening issue in diabetes. Learn about its progression, screening methods, and advanced treatments, all aimed at protecting vision in the face of diabetes challenges.
The prevalence of diabetes is predicted to be around 783 million by the year 2045 and is currently at 537 million as per estimates from 2021. As the incidence of diabetes is rising so does the incidence of its complications.
Diabetic retinopathy (DR) stands as one of the most prevalent and debilitating complications of diabetes mellitus (DM) along with another complication involving the macula resulting in diabetes macular oedema (DME), significantly impacting global public health.
As diabetes progresses, the elevated levels of glucose in the bloodstream can lead to damage in the tiny blood vessels nourishing the retina, initiating a cascade of pathological changes that can culminate in vision impairment and blindness if left unchecked. One-third of patients with diabetes have diabetic retinopathy. The DR prevalence according to the type of diabetes is estimated to be around 54%-77% in type 1 and 25%-52% in type 2 diabetes.
The hallmark of diabetic retinopathy lies in its insidious onset and asymptomatic early stages, often evading detection until irreversible damage has occurred. However, as the disease advances, symptoms such as blurred vision, floaters, and eventual vision loss may manifest, posing substantial challenges to affected individuals' quality of life.
Diabetic retinopathy is commonly asymptomatic and its classification is crucial for standardising diagnosis, assessing disease severity, guiding treatment decisions, and facilitating communication among healthcare professionals.
Risk factors for DR include high blood glucose, high blood pressure and high cholesterol levels. A patient may be asymptomatic with visual acuity mostly normal. Transient changes in visual acuity may occur due to variations in blood glucose levels. The better the control of diabetes, the lesser the visual changes. Typically no treatment is required unless the patient develops severe stages of non-proliferative diabetic retinopathy or diabetic macular oedema.
Early Treatment Diabetic Retinopathy Study (ETDRS) classification: This classification system, developed by the Early Treatment Diabetic Retinopathy Study, categorises diabetic retinopathy into several stages based on severity:
- No apparent retinopathy (No DR): Absence of any visible abnormalities in the retina.
- Mild non-proliferative diabetic retinopathy (NPDR): Presence of microaneurysms only.
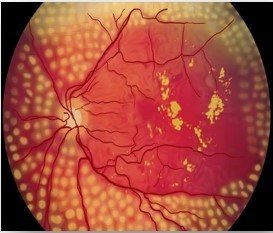
- Moderate NPDR: Presence of microaneurysms plus more than just microaneurysms but less than severe NPDR.
- Severe NPDR: Any of the following: more than 20 intraretinal haemorrhages in each of the four quadrants, definite venous beading in two or more quadrants, and/or prominent intraretinal microvascular abnormalities in one or more quadrants.
- Proliferative diabetic retinopathy (PDR): Presence of neovascularisation, characterised by the growth of abnormal blood vessels on the retina or optic disc.
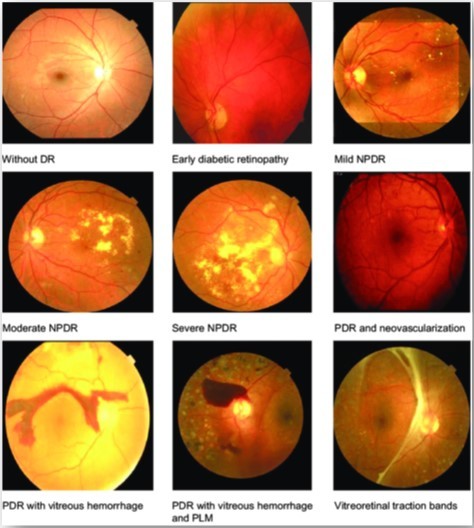
Stages of retinopathy
Diabetic macular oedema (DME)
It is a complication of diabetes that affects the eyes. It occurs when the blood vessels in the retina (the light-sensitive tissue at the back of the eye) leak fluid, causing swelling in the macula, which is the central part of the retina responsible for sharp, central vision. DME is usually symptomatic. Suddenly decreased visual acuity and problems in near or central vision. Long duration of DME with more than 6 months is associated with permanent visual impairment.
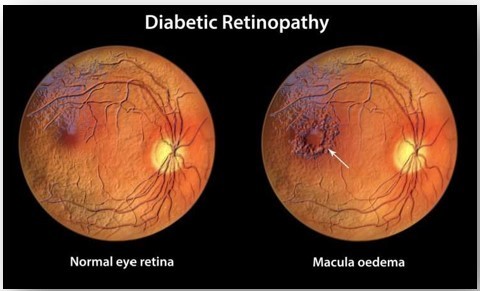
Diabetic macular oedema
When and how to do screening
As per recommendation from the American diabetes association adults with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the onset of diabetes.
People with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of the diabetes diagnosis.
Individuals with preexisting type 1 or type 2 diabetes should receive an eye exam before pregnancy and in the first trimester and should be monitored every trimester and for 1 year postpartum as indicated by the degree of retinopathy.
The examination needs to be more frequent if there is a fast progression of retinopathy.
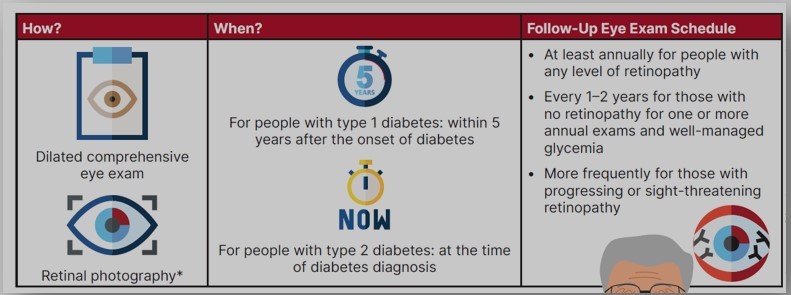
Screening schedule for diabetic retinopathy
Management of diabetic retinopathy
The first and foremost is to implement strategies to help people with diabetes reach glycemic goals along with blood pressure and lipid goals to reduce the risk or slow the progression of diabetic retinopathy. The patient with any level of diabetic macular oedema, moderate or worse non-proliferative diabetic retinopathy (a precursor of proliferative diabetic retinopathy [PDR]), or any PDR should be referred to an ophthalmologist. Aspirin therapy is not contraindicated for individuals with retinopathy, as it does not increase the risk of retinal haemorrhage.
The treatment options for diabetic retinopathy are:
Anti-vascular endothelial growth factor (anti-VEGF) therapy: Anti-VEGF medications, such as ranibizumab, aflibercept, and bevacizumab, are commonly used to treat diabetic macular oedema (DME) and proliferative diabetic retinopathy (PDR). These medications work by blocking the action of VEGF, a protein that promotes abnormal blood vessel growth and leakage in the retina. Anti-VEGF injections are typically administered directly into the eye (intravitreal injections) and may require regular monitoring and retreatment to maintain efficacy.
Laser photocoagulation: Laser photocoagulation therapy, such as focal/grid laser treatment or pan-retinal photocoagulation (PRP), may be used to treat proliferative diabetic retinopathy and diabetic macular oedema by sealing leaking blood vessels, reducing oedema, and preventing the growth of abnormal blood vessels in the retina. However, its use has declined with the advent of anti-VEGF therapy, as it may cause visual field loss and other complications.
Steroid therapy: In cases of refractory diabetic macular oedema or non-responsiveness to anti-VEGF therapy, corticosteroids may be used to reduce inflammation and oedema in the retina. Intravitreal corticosteroid injections or sustained-release implants (such as dexamethasone implants) may be considered as alternative or adjunctive treatments.
Vitrectomy: In advanced cases of proliferative diabetic retinopathy with significant vitreous haemorrhage or tractional retinal detachment, vitrectomy surgery may be necessary to remove blood and scar tissue from the vitreous cavity, repair retinal tears, and restore vision.
Conclusion
Diabetic retinopathy is a serious complication of diabetes that can lead to vision loss if not properly managed. However, with proper glycemic control along with blood pressure goals and lipid goals and regular eye exams and early detection, the progression of diabetic retinopathy can be slowed, vision loss can be prevented or minimised.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries