Diabetic Dyslipidemia in the Indian Population
M3 India Newsdesk Apr 12, 2023
Patients with diabetes are at 1.5- 2 fold higher risk of Atherosclerotic cardiovascular disease (ASCVD) when compared to nondiabetic patients. Key recommendations from different guidelines for the management of diabetic dyslipidemia along with the treatment are discussed in this article.
As of the latest data, the prevalence of CAD in India was estimated at 21.4% among those with diabetes and 11% among non-diabetics. Diabetic dyslipidemia is very common and it is a cluster of lipoproteins abnormalities typically characterised by a triad which consists of an increase in triglyceride levels, an increase in small dense low-density lipoprotein (LDL) particles along with a decrease in high-density lipoprotein (HDL). This article will give physicians insight into the treatment of diabetic dyslipidemia as per the latest recommendation from the Lipid Association of India (LAI), the American Diabetic Association (ADA) and various societies.
Objectives of the recommendation are to reduce cardiovascular morbidity and mortality in patients of Indian origin with diabetes.
The 2 major consequences of diabetic dyslipidemia are:
- Premature ASCVD from the elevated apo-lipoprotein B-carrying particles.
- Pancreatitis with severe HTG > 1000 mg/dL.
Key recommendations from different guidelines
As per the Lipid Association of India;
- Patients with diabetes and no ASCVD, no target organ damage and having ≤1 risk factor are designated as high risk and an LDL-C goal <70 mg/dl is recommended.
- Patients with diabetes and no ASCVD, with target organ damage or having ≥2 risk factors are designated as very high risk and an LDL-C goal <50 mg/dl is recommended.
- Patients with diabetes and ASCVD, with target organ damage along with other risk factors like stroke, are considered designated as an extreme risk category requiring aggressive LDL-C management and an LDL-C goal of ≤30 mg/dl is recommended.
As per the American Association of Clinical Endocrinologists guidelines;
- Patients with high risk [≥ 2 risk factors and 10-year risk 10%-20%, or chronic kidney disease (CKD) stage 3-4 with no other risk factors], should be treated for LDL targets of < 100 mg/dl.
- Patients with very high risk [established acute coronary syndrome (ACS) or recent hospitalisation for ACS, peripheral arterial disease, carotid, coronary artery disease, 10-year risk ≥ 20%, CKD stage 3-4 with 1 or more risk factors, heterozygous familial hypercholesterolemia], should be treated for LDL targets of < 70 mg/dl.
- Patients with extremely high risk (progressive ASCVD, coronary artery disease with CKD stage 3-4, diabetes or heterozygous familial hypercholesterolemia, history of premature ASCVD in females age < 65 or males with age < 55 years) should be treated for LDL targets of < 55 mg/dL.
As per American Diabetes Association guidelines;
- Primary prevention with statin therapy is recommended only in patients with diabetes at an age of 40 years or older.
- Patients with ASCVD or patients with a 10-year atherosclerotic cardiovascular risk > 20% should be treated with high-intensity statins (goal of 50% reduction in LDL-cholesterol) in addition to lifestyle modification.
- Diabetic patients aged < 40 with additional atherosclerotic cardiovascular risk factors (LDL-C ≥ 100 mg/dL, hypertension, CKD, smoking, albuminuria and FH of premature ASCVD) should be treated with moderate-intensity statins with a goal of 30%-49% LDL-C reduction.
- Diabetic patients aged 40-75 years without ASCVD or 10-year ASCVD risk < 20% and diabetic patients > 75 years old should be treated with moderate-intensity statins with a goal of 30%-49% LDL-C reduction.
As per ACC/AHA guidelines;
Patients with diabetes are defined as having high-risk conditions for ASCVD. ACC has also provided diabetes-specific risk enhancers which include:
- Diabetes duration of >10 years in T2DM and >20 years duration for T1DM
- Albuminuria > 30 mg/G creatinine and an eGFR < 60 mL/min /1.73m2
- Retinopathy, neuropathy and an ankle-brachial index (ABI) < 0.9
In adults 40-75 years with diabetes regardless of 10-year risk initiate moderate-intensity statin. In adults 40-75 years old with LDL-C between 70-189 mg/dl without ASCVD the 10-year risk should be assessed, if the risk is 20% or higher, then the treatment should aim for an LDL-C reduction of 50% or greater. For patients with diabetes between 20-39 years of age, it is reasonable to institute moderate-intensity statin therapy if the above-mentioned diabetes-specific risk enhancer is present.
Diagnosis
As per recommendations for routine screening, a fasting lipid profile is not mandatory but a fasting profile should be considered at a second visit especially in Indian patients before starting treatment for hypercholesterolemia. Genetic testing can be considered in patients with a history of familial hypercholesterolemia. Non-HDL-C should be calculated in individuals by subtracting HDL-C from total cholesterol and representing the sum of all circulating atherogenic lipoproteins including LDL, remnant lipoproteins, and lipoprotein. Lipids should be checked every three months or more frequently when necessary.
Treatment
The goal of treatment for dyslipidemia in diabetes requires attention to all aspects of atherogenic dyslipidemia with an additional focus on lowering LDL-C. The treatment can be divided into non-pharmacological and pharmacological treatment.
Non- pharmacological treatment: It consists of lifestyle modification which includes medical nutrition therapy, physical activity and weight loss. As per guidelines, for every diabetic patient lifestyle modification must be advised primarily before considering pharmacological treatment.
As per recommendation, a diabetic patient should engage in at least 150 min per week of total moderate-intensity or 75 min per week of vigorous-intensity aerobic physical activity. Around 5-7% weight loss is associated with improvement in glycemic control, insulin resistance and improvement in lipid profile. As per data weight loss helps in decreasing triglyceride levels and raises HDL-C levels.
Diabetic patients should be advised to increase the intake of plants based diet, viscous fibre, and omega-3 fatty acids and decrease the intake of trans-fatty acids and saturated fatty acids. ADA recommends the Mediterranean diet or DASH (Dietary Approaches to Stop Hypertension) diet, Tree nuts, peanuts, and grains.
Pharmacological treatment: It consists of lipid-lowering drugs which include statins, bempedoic acid, cholesterol absorption inhibitors, niacin, fibrates, bile acid sequestrants (BAS), PCSK9 inhibitors, omega-3 fatty acids and saroglitazar.
- Statin - First-line agent for lowering lipids is a statin, regardless of the therapeutic target. Increasing the dosage of statin or switching to a more potent statin and intensifying lifestyle measures should be the first step to achieving further non-HDL- C lowering, even when the LDL-C goal has been achieved. Atorvastatin is the most potent triglyceride-reducing statin. Simvastatin at a dose of 80 mg daily can also lower triglyceride, but this dose may increase adverse effects associated with statin use.
- Fibrates - The major indication of fibrates (fenofibrate, bezafibrate and gemfibrozil) is to reduce triglyceride in patients with very high TG who are at risk for pancreatitis. Briefly, in patients with severe HTG > 1000 mg/dL, secondary causes such as excess alcohol intake, drugs (steroids, oral estrogen, protease inhibitors etc.,) and kidney disease should be ruled out. Good glycemic control can help in reducing the level of triglycerides. Maintain triglycerides <150 mg/dl through lifestyle modification and medicine.
- Bempedoic Acid - A new drug which significantly lowers LDL-C across glycemic strata and did not worsen the glycemic variables. This drug is helpful in patients who cannot tolerate statins or have severe side effects due to the use of statins.
- Ezetimibe - This drug inhibits the absorption of cholesterol from the small intestine and can be added along with statins in patients who are not able to achieve the LDL targets even after the maximum tolerated dose of statin.
- PCSK-9 inhibitors - These are the new class of drugs that lowers the LDL-C in statin-tolerant patients and are indicated in patients with familial hypercholesterolemia. Evolocumab, alirocumab and inclisiran are a few examples of pcsk-9 inhibitors.
- Saroglitazar - This is the drug approved by DCGI for the treatment of type 2 diabetes mellitus and dyslipidemia mainly hypertriglyceridemia. This drug acts as a dual PPAR agonist which helps in lowering high blood TG through PPAR alpha along with reducing blood glucose levels through PPAR gamma receptors.
- Omega-3 fatty acids - These are sometimes used as add-on therapy to reduce triglyceride levels. Some experts do not recommend them.Omega-3 fatty acid formulations contain eicosapentaenoic acid (EPA) and docosahexaenoic acid.
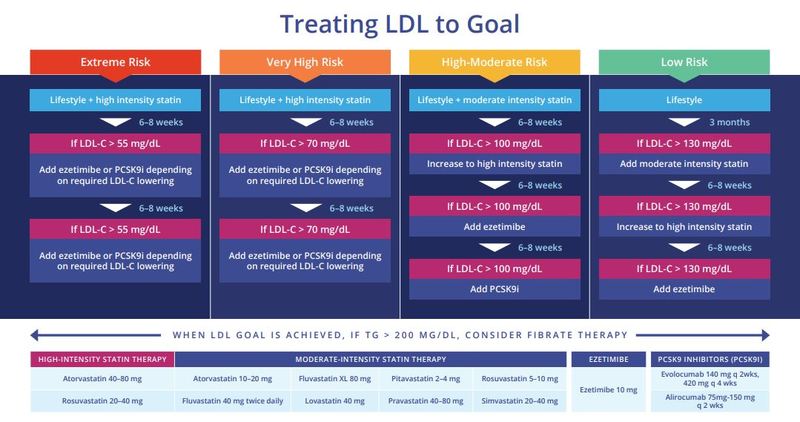 ACCE (2020) algorithm to treat LDL-C
ACCE (2020) algorithm to treat LDL-C
Conclusion
Due to the higher risk of ASCVD in diabetic patients along with the risk of early onset of ASCVD observed in Indians, it becomes important for physicians to start the treatment of diabetic dyslipidemia as early as possible. When diagnosed with diabetes the lipid targets of LDL-C, non-HDL-C and Apo b should be achieved based on the ASCVD risk category. The patients should be counselled about the role of lifestyle modification to achieve the lipid targets along with control of diabetes. Statins remain the primary pharmacological intervention for diabetic dyslipidemia. With the advent of new drugs like bempedoic acid, and PCSK inhibitors achieving lipid targets is very well possible.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries