Cushing's Syndrome: An Overview of Management
M3 India Newsdesk Oct 18, 2023
This article provides an overview of Cushing's syndrome, emphasising the importance of a thorough evaluation to determine the underlying aetiology and formulate effective treatment strategies.
Case presentation
- A 4-year-old girl presented to the endocrinology op with weight gain and lethargy for 3 months.
- She had a recent episode of sudden onset headache with vomiting and loss of consciousness and was taken to a local hospital.
- She was found to have accelerated hypertension 160/100 mm of Hg. She was managed with injectable antihypertensives. She is presently on labetalol and amlodipine.

Figure 1: 4-year-old with moon facies, hypertrichosis, facial plethora
How do we approach this patient?
Introduction
Cushing's syndrome (CS) is a condition comprising symptoms and signs that occur due to prolonged exposure to glucocorticoids that can be endogenous or exogenous. The most common cause of CS is due to iatrogenic exogenous glucocorticoid intake. Endogenous causes are rare comprising 2-8 cases per million annually.
Aetiology of Cushing’s syndrome
Exogenous CS is the most common cause due to prolonged exposure to glucocorticoids.
Endogenous CS can be classified into:
A. ACTH dependent CS
- Cushing’s disease (accounts for almost 70% of endogenous CS)
- Ectopic ACTH secretion
- Lung carcinoma
- Neuroendocrine/carcinoid tumours of the lung, thymus and pancreas
- Pheochromocytoma and paraganglioma
- Medullary carcinoma of the thyroid
- Rare carcinomas of prostate, breast, ovary, gallbladder, colon
- Ectopic CRH secretion
B. ACTH independent CS
- Adrenal adenoma
- Adrenal carcinoma
- Primary Pigmented Nodular Adrenal Disease (PPNAD) and Carney complex
- McCune-Albright syndrome (MAS)
- ACTH Independent Macronodular Adrenal Hyperplasia
C. Other causes of hypercortisolism
- Alcohol
- Pregnancy
- Depression
- Obesity
In the pediatric age group adrenal causes of CS is more common accounting for almost 65% of the cases.
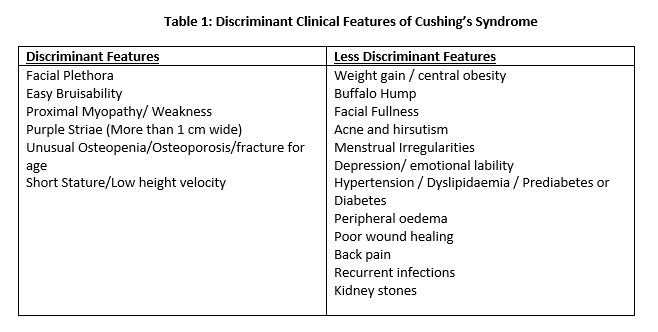
Clinical features of Cushing’s syndrome
The classical features of CS are not always present in all patients and it requires a careful history and examination with a high degree of suspicion.
Symptoms
The symptoms and signs are variable and it is dependent on many factors:
- The duration of exposure to glucocorticoids.
- The severity of glucocorticoid excess.
- Aetiology of Cushing's – ACTH-dependent tumours usually have hyperpigmentation.
- Age of onset - Children usually present with generalised obesity, short stature and depressed mood whereas adults have central obesity.
Diagnosis
Always take a detailed history of exogenous glucocorticoid intake prior to starting evaluation of Cushing’s syndrome.
Who should be tested?
- Patients with multiple and progressive features, particularly those who are more predictive of Cushing’s syndrome.
- Children with decreasing height percentile and increasing weight.
- Patients with adrenal incidentaloma compatible with adenoma.
- Patients with unusual features for age (e.g. osteoporosis, hypertension).
Screening tests
- Urine-free cortisol (UFC; at least two measurements)
- Late-night salivary cortisol (two sizes)
- 1-mg overnight dexamethasone suppression test (DST)
- Longer low-dose DST (2 mg/day for 48 h)
If any of the screening tests are positive one should proceed to do another screening test. If both screening tests are abnormal then this confirms endogenous Cushing’s syndrome.
Determining the aetiology of Cushing’s syndrome
- Plasma ACTH – Detectable or high levels (More than 15pg/ml) suggest ACTH-dependent CS whereas ACTH will usually be suppressed (Less than 5pg/ml) in ACTH-independent causes.
- High Dose Dexamethasone Suppression Test (HDDST) and Corticotrophin-Releasing Hormone (CRH) Stimulation Test help in the diagnosis of ACTH Dependent CS due to pituitary causes.
- Inferior Petrosal Sinus Sampling (IPSS) helps the differentiation of Ectopic ACTH secretion from Cushing’s disease.
The approach is summarised in Figure 2
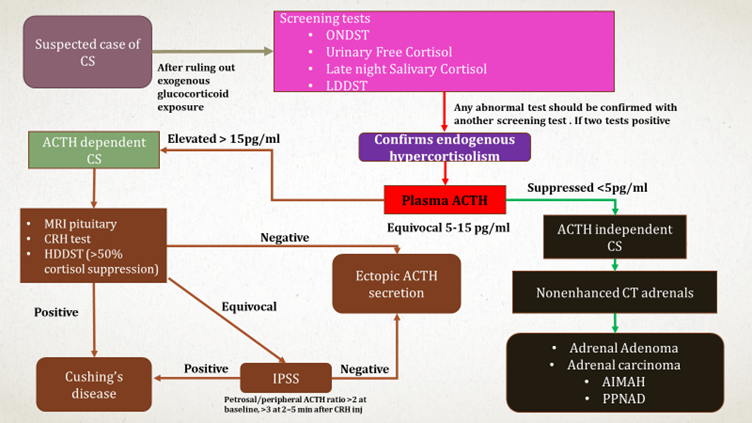
Figure 2: Approach to Cushing’s syndrome
Imaging
- MRI Pituitary or CT/MRI Adrenals
- Somatostatin Scintigraphy or DOTATATE PET CT
Management of Cushing's syndrome
The main goals of management are:
- Normalisation of cortisol secretion.
- Reversal of clinical picture.
- Prevention or recovery of the concomitant comorbidities and complications.
- Long-term disease control without recurrence.
Treatment modalities include surgical, medical or radiotherapy. The choice of therapy depends on the aetiology of CS. In neoplastic aetiology, surgery is the 1st line of treatment.
Surgical- For Cushing’s disease due to pituitary causes, transphenoidal Surgery is the treatment of choice. In the case of adrenal adenoma or carcinoma, unilateral adrenalectomy is the preferred treatment.
Radiotherapy- Conventional or stereotactic radiation (Gamma knife, proton beam or linear accelerator) can be used in case of recurrence.
Medical Management- It is used to reduce hypercortisolemia prior to surgery as second-line treatment in recurrent CS, in inoperable patients or while awaiting the benefit of radiotherapy. These include:
- Pituitary-directed drugs – Pasreotide, cabergoline, temozolomide
- Steroid synthesis inhibitors – Ketoconazole, etomidate, mitotane, metyrapone
- Glucocorticoid receptor antagonists - Mifepristone
- Combination therapy
Bilateral adrenalectomy is used very rarely. It is indicated in the following:
- 1. Very severe ACTH-dependent CS needing rapid resolution of hypercortisolism
- 2. Occult or metastatic Ectopic ACTH Secretion not controlled by medical therapy
- 3. PPNAD
Adjunctive treatment in CS
- Thromboembolism prophylaxis - Low Molecular Weight Heparin
- Infection - Pneumocystis jirovecii prophylaxis
- Hypopituitarism - Adequate hormone replacement
- Diabetes - Mifepristone and cabergoline improve glycemia, Pasireotide-induced dysglycemia - Metformin, DPP4, GLP1 or insulin
- Dyslipidemia
- Rosuvastatin and pravastatin for mitotane - Induced dyslipidaemias
- Hypertension - ACE inhibitors or ARB are preferred
- Osteoporosis - Calcium + Vit D3, bisphosphonates, teriparatide or denosumab
On examination
- Her pulse was 80/min (regular) and her blood pressure was 124/74mm Hg (> 95th centile)
- Her height was 96cm (3-10th centile), weight- was 26kg (>97th centile)
- BMI was 28.2 kg/m2 (>95th centile)
- She had moon facies, facial plethora, hypertrichosis and depressed mood (Figure 1)
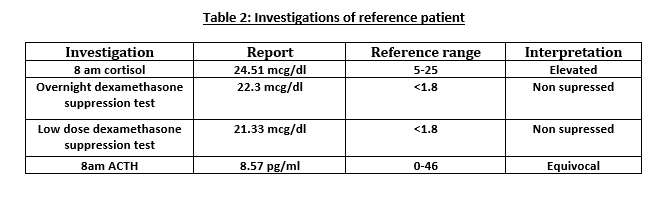

Figure 3: CT Abdomen showing right adrenal mass

Figure 4: Right adrenalectomy and specimen photo
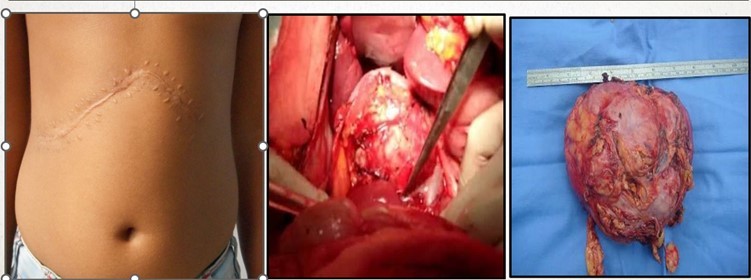
(Sensitive content- Click on the image to view)
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Rahul Valsaraj is an Associate Consultant, at the Department of Endocrinology, VPS Lakeshore Hospital, Kerala.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries