COVID-19 & seasonal illness- Protocol for determining co-infection
M3 India Newsdesk Jun 29, 2021
The seasonal pattern of epidemic-prone diseases observed each year includes several diseases. Going forward, these diseases will coexist with the ongoing COVID-19 pandemic and can also bring about a number of clinical and laboratory diagnostic issues. This article, a part of our new series- COVID-19 co-infections will throw light on the behaviour pattern and diagnostics of seasonal diseases co-existing with the pandemic.
For our comprehensive coverage and latest updates on COVID-19 click here.
Introduction
COVID-19 has touched almost all of the country's states and territories. Illnesses like dengue, malaria, seasonal influenza, leptospirosis, chikungunya, enteric fever, and others might not only offer a diagnostic difficulty but also co-exist in COVID patients, given the seasonal pattern of epidemic-prone diseases found every year in our country. This complicates COVID clinical and laboratory diagnosis, with implications for clinical care and patient outcomes. The purpose of this article is to offer clear guidance for COVID co-infections with illnesses such as dengue, malaria, seasonal influenza (H1N1), leptospirosis, chikungunya, and others.
Characteristics of seasonal epidemic-prone disorders
Acute onset of fever and cough or acute onset of any three or more of the following signs or symptoms, according to the World Health Organization (WHO) case definition:
- Fever
- Cough
- General weakness/fatigue
- Headache
- Myalgia
- Sore throat
- Coryza
- Dyspnoea
- Anorexia/nausea
- Vomiting
- Diarrhoea
- Altered mental status
Although sensitive, this case definition is not extremely explicit. Seasonal epidemic-prone disorders, such as those listed above, can all appear as a febrile illness with symptoms that are similar to COVID-19. If there is a co-infection, there may be a constellation of signs and symptoms in addition to the febrile sickness, making diagnosis more complex.
Protocol for determining the presence of a suspected co-infection
For epidemic-prone illnesses, (e.g., dengue, malaria, chikungunya, seasonal influenza, leptospirosis) common in a specific geographic region throughout the monsoon and post-monsoon seasons, a high index of suspicion must be maintained. In moderate or severe instances of COVID-19 that do not respond to therapy, bacterial co-infections must also be considered.
Malaria/Dengue: Because malaria/dengue can coexist with other illnesses, confirmation of malaria/dengue infection does not rule out the likelihood that the patient does not have COVID-19. Similarly, when a fever case is classified as COVID-19, a high index of suspicion of malaria/dengue must be present, especially during the rainy and post-rainy seasons in places endemic for these illnesses.
Seasonal influenza: Because both COVID-19 and seasonal influenza cause influenza-like illness (ILI/SARI), all ILI/SARI patients in locations where COVID-19 cases have been reported must be investigated and tested for both COVID-19 and seasonal influenza if both viruses are prevalent in the population.
Chikungunya: Chikungunya is characterised by an initial onset of moderate to high fever and malaise, which is followed by a rash, myalgia, and arthralgia. In the late stages, respiratory failure may occur. In Chikungunya-endemic locations, co-infection with COVID-19 is possible during the monsoon season.
Leptospirosis: In addition to presenting as a febrile sickness, leptospirosis can also appear as an acute respiratory sickness, resulting in respiratory distress and shock. Coinfection should be considered in locations where leptospirosis epidemics are known to occur during the monsoon/postmonsoon.
Scrub typhus: Scrub typhus is common in the Himalayan foothills, including Jammu and Kashmir, Himachal Pradesh, Sikkim, Manipur, Nagaland, and Meghalaya. Scrub typhus outbreaks have also been documented in Delhi, Haryana, Rajasthan, Maharashtra, Uttarakhand, Chhattisgarh, Tamil Nadu, and Kerala in the recent past. A rapid high-grade fever, severe headache, lethargy, myalgia, and widespread lymphadenopathy characterise the clinical presentation. Within a few days, a maculopapular rash may form on the trunk, then spread to the limbs and blenches. Interstitial pneumonia (30 to 65 per cent of the time), meningoencephalitis, and myocarditis are also possible consequences. COVID-19 and scrub typhus infection may coexist.
Bacterial infections: A subsequent bacterial infection is uncommon in COVID-19 patients. Empiric antibiotic treatment based on the local antibiogram should be explored in such circumstances.
Despite the probability of the aforementioned co-infections, the methodology to diagnosis for COVID-19 remains roughly the same in the current epidemic. The testing methodology will be conducted in accordance with the MoHFW/ICMR recommendations. However, anytime a possible co-infection is detected, more testing will be performed.
Diagnostics
Even when many of these infections are antigenically distinguishable, with distinct serological responses, in the event of co-infections, cross-reactions (resulting in false-positive/false-negative results) cannot be completely ruled out, especially if the testing kits used to lack the necessary sensitivity and specificity. As a result, the ICMR's (for COVID-19) and the concerned programme divisions' (NVBDCP for vector-borne illnesses [malaria, dengue, chikungunya]) and NCDC (seasonal influenza, leptospirosis, scrub typhus) recommendations must be implemented. Rapid diagnostic tests for malaria, dengue fever, and scrub typhus should be available at such COVID treatment centres.
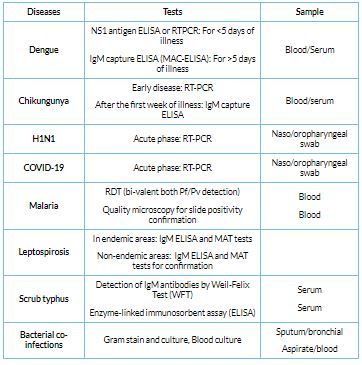
The table below lists the numerous (confirmatory) tests that should be performed to rule out suspected coinfections.
Laboratory testing: Other seasonal epidemic-prone illnesses coinfected with COVID 19
This article is part of our new series on managing COVID-19 coinfections. Stay tuned for a new update every Tuesday.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries