COVID-19 in children and adolescents (below 18 years): Management guidelines by MoHFW
M3 India Newsdesk Jul 13, 2022
The dynamic guidelines for COVID-19 management in children and adolescents (below 18 years) by MoHFW are elucidated in this article.
The committee of specialists revised the Comprehensive Guidelines for Management of COVID-19 in children and adolescents (below 18 years) in light of the present increase, which is mostly attributable to the Omicron variation of concern.
The available data from other nations shows that the sickness induced by the Omicron variation is less severe; nonetheless, it is necessary to keep a close eye on the evolution of the present wave. These recommendations are dynamic and will be reviewed and revised when new data becomes available.
The specialists have evaluated the available evidence and, with the exception of a few modifications detailed below
- Regardless of the severity of the illness, the use of antivirals or monoclonal antibodies is not advised for children under 18 years old.
- Regarding the diagnosis of MIS-C, care must be used when interpreting an isolated rise in COVID antibodies.
- The new CRP threshold for diagnosing MIS-C is >5 mg/dL.
- The use of corticosteroids should be decreased over a period of 10 to 14 days, pending clinical improvement.
- The use of anticoagulants has been modified.
- Addition of a new section on post-COVID care.
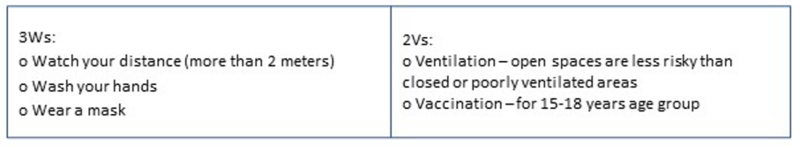
COVID appropriate behaviour
COVID appropriate behavior is advised for the prevention of SARS-CoV-2 infections:
Asymptomatic cases
-Positive without symptoms.
Treatment:
- Home isolation.
- Infants and children under parent's care.
- No specific drug therapy.
- Continue medications for other conditions.
- Promote COVID appropriate behaviour.
- Fluids and feeding for proper hydration and nutrition.
- Older children stay connected for positive talks through phone, and video.
Investigations:
Not needed.
Mild cases
-Sore throat, cough without breathing difficulty; SpO2 >94% room air
Treatment:
- Home isolation.
- For fever , paracetamol 10-15 mg/kg/dose every 4-6 hrs.
- For cough, give throat soothing agents, and warm saline gargles to older children.
- Fluids and feeding for proper hydration and nutrition.
- No specific drug therapy.
- Monitoring – respiratory rate, chest indrawing, urine output, cold extremities, activity level.
- Promote COVID-appropriate behaviour.
- Older children – stay connected for positive talks through phone, or video.
- In case of deterioration of symptoms, contact the physician.
Investigations:
Not needed.
Moderate cases
-In addition to symptoms of mild cases check for pneumonia which may not be apparent.
- Rapid respiration- <2 months – RR>60/min
- 2-12 months – RR >50/min
- 1-5 yrs – RR > 40 /min
- >5 yrs – RR >30/min
- And/or SpO2 90-93%room air
Treatment
- Admit to COVID hospital.
- Initiate oxygen if spo2 <94%.
- Maintain fluid and electrolyte balance.
- Steroids not needed in moderate cases may be administered in rapidly progressive diseases.
- Fever >38 C/ 100.4 F- paracetamol 10-15 mg/kg/dose every 4-6 hrs.
- Antimicrobials to be administered if there is evidence of superadded bacterial infections.
- Supportive care for comorbid conditions.
Investigations
- Baseline CBC, ESR, Blood glucose
- CXR
Severe Cases
- SpO2 < 90% room air
- Any of the following – severe pneumonia, ARDS, Septic shock, MODS, cyanosis, grunting, retraction of the chest
Treatment:
- Admit to COVID hospital.
- Initiate oxygen to maintain spO2 94-96%.
- Maintain fluid and electrolyte balance.
- Steroid therapy should be initiated.
- Anticoagulants may also be indicated.
- Antimicrobials to be administered if there is evidence of superadded bacterial infections.
- Supportive care for comorbid conditions.
- In the case of ARDS, initiate appropriate management.
- May need Organ supportive care e.g. RRT.
Investigations
- Baseline CBC, ESR, Blood glucose, CRP, LFT KFT D dimer.
- CXR
Management of acute respiratory distress syndrome (ARDS) and shock guide:
Based on the Pediatric Acute Lung Injury Consensus Conference (PALICC) classification, ARDS may be classed as mild, moderate, or severe.
i) Mild ARDS
- High flow nasal oxygen (start with 0.5 L/kg/min, to begin with and increase to 2 L/kg/min with monitoring) or non-invasive ventilation (BiPAP or CPAP) may be given.
ii) Moderate-Severe ARDS
- Lung protective mechanical ventilation may be initiated, low tidal volume (4-8 ml/kg); plateau pressure <28-30 cmH2O, MAP <18-20 cmH2O; driving pressure <15 cmH₂0; PEEP 6-10 cm H₂0 (or higher if severe ARDS), FiO2, <60% sedoanalgesia ± neuromuscular blockers; cuffed ETT, inline suction, heat and moisture exchange filters (HMEF).
- Avoid frequent disconnection of the ventilator circuit, nebulisation or metered-dose inhaler.
- Restrict fluids; calculate fluid overload percentage, keeping it <10%.
- Prone position may be considered in hypoxemic children if they are able to tolerate it.
- Daily assessment for weaning and early extubation; enteral nutrition within 24 hours, achieve full feeds by 48 hours.
- Transfusion trigger Hb <7g/dL if stable oxygenation and hemodynamics and <10 g/dL if refractory.
- hypoxemia or shock.
Management of shock:
- Consider crystalloid fluid bolus 10-20 ml/kg cautiously over 30-60 minutes with early vasoactive support (epinephrine).
- Start antimicrobials within the first hour, after taking blood cultures, according to hospital antibiogram or treatment guidelines.
- Consider inotropes (milrinone or dobutamine) if poor perfusion and myocardial dysfunction persist despite fluid boluses, vasoactive drugs and achievement of target mean arterial pressure.
- Hydrocortisone may be added if there is fluid refractory catecholamine resistant shock (avoid if already on dexamethasone or methylprednisolone).
- Once stabilised, restrict IV fluids to avoid fluid overload.
- Initiate enteral nutrition-sooner the better.
- Transfusion trigger Hb <7g/dL if stable oxygenation and hemodynamics, and <10 g/dL if refractory hypoxemia or shock.
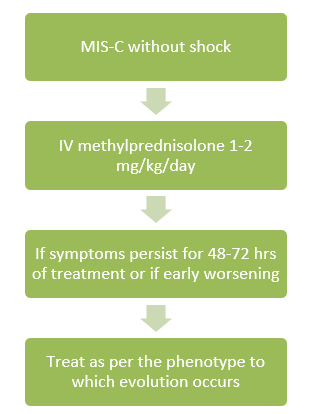
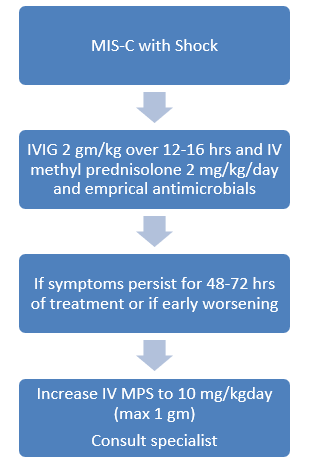
Management of multisystem inflammatory syndrome (MIS-C) in children and adolescents temporally related to COVID-19
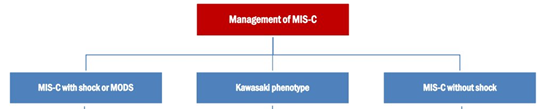
Multi-system inflammatory syndrome in children (MIS-C) is a new syndrome in children characterised by unremitting fever >38°C and epidemiological linkage with SARS-CoV-2.
Diagnostic criteria (WHO) - Children and adolescents (0-18 years of age) with fever ≥3 days and any two of the following:
- Rash or bilateral non-purulent conjunctivitis or mucocutaneous inflammation signs (oral, hands or feet).
- Hypotension or shock.
- Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities (including ECHO findings or elevated Troponin/NT-proBNP).
- Evidence of coagulopathy (PT, PTT, elevated D-Dimers).
- Acute gastrointestinal problems (diarrhoea, vomiting, or abdominal pain.
- And elevated markers of inflammation such as ESR (>40 mm), C-Reactive Protein (>5 mg/dL), or procalcitonin.
- And no other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes.
- And evidence of recent COVID-19 infection (RT-PCR antigen test or serology positive), or likely contact with patients with COVID-19.
Alternative diagnoses that must be excluded before making a diagnosis of MIS-C
- Tropical fevers (malaria, dengue, scrub typhus, enteric fever)
- Toxic shock syndrome (staphylococcal or streptococcal)
- Bacterial sepsis
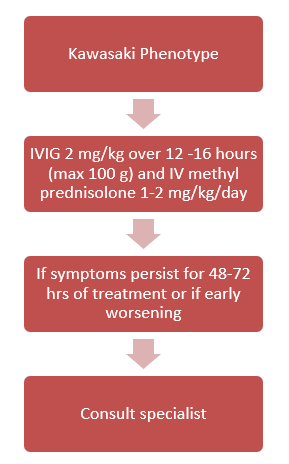
MIS-C with Kawasaki Disease (KD)
MIS-C with Kawasaki Disease (KD) phenotype is characterised by fever, conjunctival redness, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet and cervical lymphadenopathy.
Appropriate supportive care is needed preferably in ICU for the treatment of cardiac dysfunction, coronary involvement, shock or multi-organ dysfunction syndrome (MODS)
- IVIG to be given slower (over up to 48 hours) in children with cardiac failure/ fluid overload.
- Taper steroids over 2-3 weeks with clinical and CRP monitoring.
- Aspirin 3-5 mg/kg/day, maximum 75 mg/day in all children for 4-6 weeks (with platelet count >80,000/μL) for at least 4-6 weeks or longer for those with coronary aneurysms.
- Low molecular weight heparin (Enoxaparin) 1 mg/kg/dose twice daily s/c in >2 months (0.75mg/kg/dose in <2 months) if the patient has thrombosis or giant aneurysm with absolute coronary diameter ≥8 mm or Z score ≥10 or LVEF <30%.
- For children with cardiac involvement, repeat ECG 48 hourly & repeat ECHO at 7–14 days and between 4 to 6 weeks, and after 1 year if initial ECHO was abnormal.
Use biologicals only after expert consultation and in tertiary care only.
Infection prevention and control (IPC)
Every COVID care facility should have a multidisciplinary hospital infection control committee; key components of infection control strategy are:
- Standard precautions
- Droplet precautions
- Airborne precautions
- Contact precautions and hand hygiene
- Physical distancing
- Cough etiquette/respiratory hygiene
- Well-ventilated rooms
- Monitor healthcare-associated infections
- Train all health care workers to develop IPC skills
Environment cleaning, disinfection, and sanitation
- Cleaning/disinfection of frequently touched surfaces/equipment
- Cleaning and disinfection of linen
- Safe management of bio-medical waste
- Triple-layer mask to be worn by the patient as per guidance below
- Masks for caregivers (home/hospital)
Guide for using the mask
- Masks are not recommended for children aged 5 years and under.
- Children aged 6-11 years may wear a mask depending on the ability of the child to use a mask safely and appropriately under the direct supervision of parents/guardians.
- Children aged 12 years and over should wear a mask under the same conditions as adults.
- Ensure hands are kept clean with soap and water, or an alcohol-based hand rub while handling masks.
Antimicrobial use guide
COVID-19 is a viral infection and antimicrobials have no role in the management of uncomplicated COVID-19 infection.
1. Asymptomatic and mild cases- Antimicrobials are not recommended for therapy or prophylaxis.
2. Moderate and severe cases- Antimicrobials should not be prescribed unless there is clinical suspicion of a superadded infection.
3. Septic shock- Empirical antimicrobials (according to body weight) are frequently added to cover all likely pathogens based on clinical judgement, patient host factors, local epidemiology and the antimicrobial policy of the hospital.
Post COVID care steroids:
1. Steroids are not indicated and are harmful in asymptomatic and mild cases of COVID-19.
2. Indicated only in hospitalised severe and critically ill COVID-19 cases under strict supervision.
3. Steroids should be used at the right time, in the right dose and for the right duration.
4. Indications and recommended doses of corticosteroids may be used in rapidly progressive moderate and all severe cases:
- Dexamethasone 0.15 mg/kg, maximum dose 6 mg once a day OR
- Methylprednisolone 0.75 mg/kg, maximum dose 30 mg once a day
5. Continue for 5-7 days and taper up to 10-14 days, depending on clinical assessment on a daily basis.
6. Avoid steroids in the first 3-5 days since the onset of symptoms as it prolongs viral shedding.
Anticoagulants:
1. Not indicated routinely.
2. All hospitalised children should be evaluated for risk of developing thrombosis and monitored for the development of thrombosis.
3. Prophylactic anticoagulant is indicated in the following circumstances (the decision to administer prophylactic anticoagulation must be balanced with the child's bleeding risk):
- Strong personal or family history of VTE, or
- An indwelling central venous line and two or more additional risk factors*, or
- Four or more risk factors*
(*Predisposing risk factors for the development of thrombosis – personal history of venous thrombotic events (VTE), family history of a first-degree relative with VTE, presence of central venous line, decreased mobility from baseline, burns, active malignancy, estrogen therapy, the flare of inflammatory disease, morbid obesity, severe dehydration, recent surgery or trauma).
4. Prophylactic dose of low molecular weight heparin (Enoxaparin): 0.5 mg/kg twice daily, till the child is discharged from the hospital.
5. On suspicion of thrombosis, confirm by appropriate investigations and start on low molecular weight heparin in therapeutic doses for a period of 12 weeks with monitoring.
6. Children already on anticoagulation therapy may continue the same unless they develop active bleeding.
7. Therapeutic dose of low molecular weight heparin (Enoxaparin): 1 mg/kg twice daily.
Post-COVID Care:
- Children with an asymptomatic infection or moderate illness should get standard treatment, immunisation (if eligible), dietary counselling, and psychological support during follow-up.
- In addition to the aforementioned, parents/caregivers of children with moderate to severe COVID should be counselled about monitoring for persistent/worsening respiratory trouble and the justifications for bringing the child back to the facility at the time of hospital release.
- Children who develop organ-specific dysfunction during hospitalisation or later should get appropriate therapy.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries