Assessment of Patient with Chronic Low Back Pain
M3 India Newsdesk Mar 06, 2023
Back discomfort can occur everywhere, from the neck to the lower spine and can result to chronic back pain. The following article discusses persistent back pain by providing probable causes, assessment protocols and therapy recommendations.
Backaches are universally common and account for the majority of attendances at orthopaedic as well as general practice clinics. In the majority of cases, these episodes are of no serious consequence; and often no specific cause can be identified. The reason this problem assumes alarming proportions is that it remains one of the single most common causes of loss of working hours.
Causes of backache
Chronic backache is one that has lasted more than 12 weeks. It could be coming from the back, or arising elsewhere and is referred to the back. In 3% of all backaches, the pain arises outside the spine and is referred to the back. This must figure in the initial evaluation of the patient.
1. Common causes of “backaches” arising outside the spine are:
- Gallstones
- Kidney stones
- Pancreatic disease
- Stomach ulcers
- Aortic aneurysms
- Uterine and ovarian disease
A few explanatory comments on similar-sounding terms would be in order, as they sometimes cause confusion are as follows :
1. Spondylosis: This refers to the very commonly occurring degeneration of the intervertebral disc and consequent changes.
2. Spondylitis: This is an uncommon inflammatory condition, predominantly affecting males, and in its end-stage results in a totally stiff spine - “the bamboo spine”.
3. Spondylolysis: This refers to an error of development in the vertebra (but rarely may be due to injury) as a result of which there is a loss of continuity in the pedicle on one or both sides.
4. Spondylolisthesis: Here one vertebra slips forward (or backwards) on the lower one.
- Spondyl- The vertebra
- Osis - Degeneration
- Itis -Inflammation
- Lysis - Discontinuity or break
- Listhesis - Slipping forward or backwards
2. Back pain arising from the back is most commonly due to inappropriate posture, prolapsed intervertebral disc, and degenerative disc (spondylosis). The age of the patient gives an indication of the likely cause.
- In the 20-40 years age group, 75% of backaches are likely to be due to disc prolapses.
- At the age of 70 years, 81% of males and 79% of females will show degenerative changes.
Investigation
Viewed from the front: The spine is a straight vertical column, and any deviation from this vertical is called “scoliosis”. This in turn may be developmental, idiopathic or secondary to some other pathology.
Viewed from the side: It is gently curved forwards (lordosis) in the neck and lower back, and backward (kyphosis) in the thoracic and sacral segments. This results in a gentle S-shape, which provides a spring-like shock-absorbing action. The column is made up of individual vertebrae, separated by a disc.
The disc: It has a lamellated jelly-like structure which is efficiently designed to disseminate stress forces from the vertical to the horizontal. It does not, by itself, act as a shock absorber in the true sense of the word.
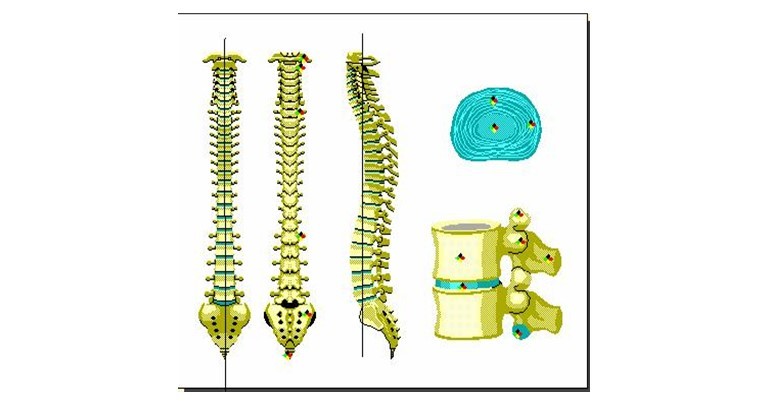
The system works most efficiently when the spine is in its optimal physiological position, namely in a plumb line viewed from the front and in a gentle S-curve when viewed from the side. This is maintained by the muscles of the back contracting to hold the individual in the optimum physiological position.
In physics, this is referred to as negative work. In the process of this negative work, the muscles generate over 40% more force/energy, which is eventually transmitted to the discs. It is easy to understand the aching in the back which results from the overworked muscles when working in a bent posture.
The disc can get squeezed out through the supportive ligaments at the back of the vertebra like toothpaste out of a tube. Degenerative changes on the other hand are a normal ageing phenomenon. These changes have a well-defined chronological sequence which can be identified anatomically and pathologically. At the age of 50 years, 95% of the population will be affected in some way or another.
Assessment of patient
The initial assessment of the patient consists of a history, clinical examination, and investigation.
History
In history, the duration of the symptoms is important. Chronic low back pain would have a longer duration and is more likely due to a degenerative condition. Following questions to be asked while taking history:
- Does it stay in the back or go down the legs?- If radiating, involvement of the nerve is suggested.
- Can you walk?- This degree of claudication gives an idea of the severity of the pain.
- Does the pain disturb your sleep?- Pain from degeneration, bad posture or a disc should improve with rest.
- Is there any tingling or numbness in the lower limbs?- This again suggests the involvement of the nerves
Examination
Clinical examinations are on the basis of the following questions:
- The examination assesses the anatomy of the spine, namely, is it straight or abnormally curved in any direction?
- Are the movements of normal range and pain-free?
- Is there any loss of sensation or muscle power?
Baseline investigations
The baseline investigations may comprise blood tests and X-rays. These provide basic information about the patient and may give an indication of the cause of the pain.
Scanning
There are two types of scans commonly in vogue; the C.T. (computerised tomography) and the M.R.I. (magnetic resonance imaging). The choice largely depends on the provisional diagnosis, availability and cost.
The more important issue is whether a scan should be done and if so when?
Before answering the question, it is important to appreciate the statistics that research has thrown up with regard to scanning disc lesions:
- 76% of patients scanned will have a demonstrable disc lesion without ever having had symptoms.
- Of these, in 40% the size of the lesion will be such as to warrant surgery judged purely from the size.
- In 30% the lesion will be incompatible with the clinical findings.
- 20% of patients will have a “normal” scan in spite of having severe symptoms.
A patient who is shown to have a disc lesion on a scan, but no symptoms can develop symptoms without any change occurring in the appearance of the disc on the scan.
The message, therefore, is that the decision to do a scan must anticipate the above facts and the inference of the scan findings has to be tempered with this knowledge. It is the clinical findings that should be the overriding factor in decision-making. For example, in the early days, if a scan showed a disc at two levels, it was acceptable to remove both. Today this is unacceptable and a surgeon is justified in operating only on the disc which correlates with the clinical signs and symptoms.
When should a scan be done?
- Certainly, where the diagnosis is in doubt.
- The patient is not responding to conservative treatment and surgery is being contemplated.
- A lesser indication would be where the patient requests it for peace of mind, to exclude serious conditions.
Treatment modalities
Finally, we must address the treatment modalities.
- The options are non-surgical or conservative treatment and surgery.
- Unless there are mitigating circumstances, a trial of conservative treatment should extend from six weeks to three months. Of this, at least five days and up to three weeks should consist of bed rest with pain-relieving medication.
- When the pain settles there should be follow-up maintenance therapy consisting of weight loss, exercises and back care/ posture training.
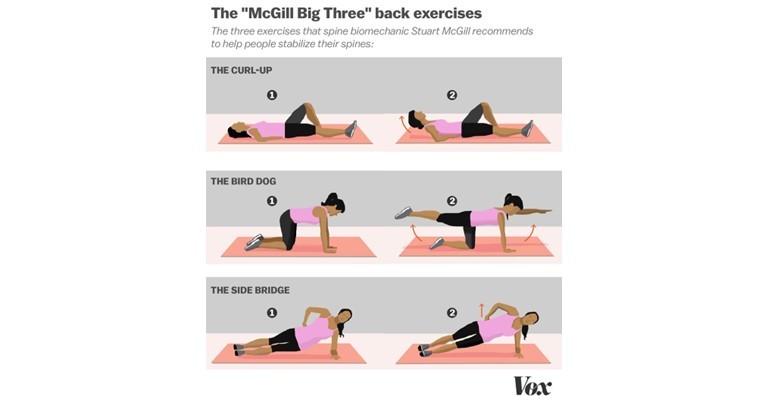
- There are many modes of treatment which have their protagonists; but there is general agreement is, that exercise remains a constant. However, there is no agreement on the type of exercise, and an example is given below.
- The emphasis is on regularity. The CDC recommends 150 minutes a week of moderate exercise.
Surgery
- Surgery is indicated when a regime of conservative treatment fails, or there is deterioration in the course of conservative treatment.
- The standard time-tested procedure was to approach the trouble spot from the back with an incision about four to six inches long. However, this has given way to minimal access surgery and endoscopic surgery.
- With special instruments, the size of the incision can be reduced. With a reduction in the size of the incision, rehabilitation is much faster.
It is important to remember that studies have shown that the results of back surgery are dependent 90% on proper patient selection and 10% on surgical expertise; with outcomes remaining at best uncertain.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Gladstone A D'Costa is an orthopaedic surgeon, currently practising at SMRC V M Salgaocar Hospital, Goa.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries