Acute Diarrhoea: Warning Signs to Watch Out for
M3 India Newsdesk Nov 03, 2023
Acute diarrhoea is a sudden & short-term episode of frequent, loose, & watery bowel movements. This article stresses the systematic assessment of acute diarrhoea, covering warning signs, causes, & evaluation methods for effective patient care.
Since acute diarrhoea is a very frequent primary care presentation, it's crucial to look for more severe pathology as well.
Most instances will be viral and resolved on their own. In these situations, hydration guidance and assurance are required. Help patients feel secure by informing them when they might anticipate their symptoms to improve. Gastroenteritis patient education pamphlets are useful.
To ensure that physicians take significant problems into account at the first evaluation, a methodical approach is necessary.
The warning signs
- More than four weeks of symptoms
- Bloody diarrhoea
- Unintentional weight loss
- Nocturnal diarrhoea
- Decreased urine production
- A history of fever
- A history of travel abroad
- A history of dining out
- Severe stomach pain
To cover all of the differential diagnoses, including acute infection, it could be helpful to go back to an undergraduate diagnostic approach.
Reasons
Acute diarrhoea
- Infections, such as viral or bacterial infections; COVID-19 may also cause diarrhoea
- Latest antibiotic usage (a higher risk of C. difficile exists)
- Iatrogenic conditions include those brought on by medications like metformin (diarrhoea is a typical adverse effect at the beginning of treatment), ischaemic colitis (ask about any history of atrial fibrillation), and diverticulosis
- Diabetes-related autonomic neuropathy
- Hepatitis A
- HIV-related disease
Chronic diarrhoea
- Colorectal cancer
- IBD
- IBS
- Thyrotoxicosis
- Other endocrine causes such as phaeochromocytoma
- Autonomic neuropathy secondary to diabetes
- Laxative abuse
- Diverticulosis
- Iatrogenic, such as NSAID-induced colitis, metformin
- Bacterial overgrowth
- Coeliac disease
- Chronic pancreatitis
- Alcoholism
- HIV and AIDS
- Bile acid malabsorption
Evaluation
- To begin with, determine precisely what the patient means by "diarrhoea," which might signify many things to various individuals.
- What occurred to the stool?
- Determine when symptoms first appeared, for instance, is this diarrhoea acute or chronic?
- What bowel habits are typical of this patient?
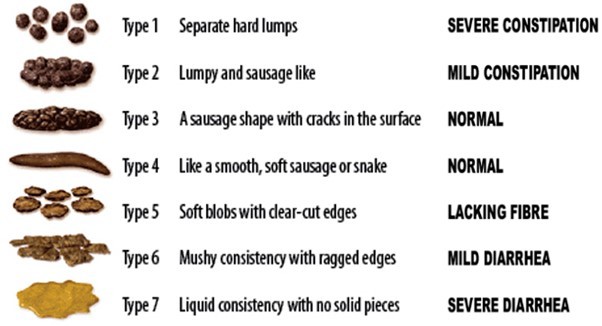
Here, the Bristol stool chart could be helpful.
Your next round of inquiries should be based on the patient's age and the sequence of events. Questions can be as follows:
- How often do they go to the bathroom and if the colour or smell of their faeces has changed?
- Asking questions like "Have they seen any blood?" and "Is there blood on the toilet paper or in the faeces?"
- Have there been any nocturnal symptoms, such as the need to defecate, that have caused them to wake up? (Nighttime symptoms should inform the doctor that the patient has inflammatory bowel disease.)
- Has this change in bowel habits been accompanied by any mucus?
- Has anybody complained of stomach pain?
- Was there any accompanying nausea or vomiting?
- Has any accidental weight loss been noticed?
- Is there any recent international travel history?
- Is there anything new about your diet or frequency of dining out?
- Have you experienced abdominal bloating?
- Does the diarrhoea become worse after eating?
Find out whether your patient has a history of constipation, and keep an eye out for constipation that causes overflow. This occurs more often in care home settings or in those who are weak.
Further queries
- Are there any other members of the household experiencing illness?
- Have they recently been admitted to the hospital or used antibiotics? Be on the lookout for possible C. difficile infections.
- Has your medicine changed in any way, or have you added any new prescription or over-the-counter medications?
- Has there been a fever that goes along with it?
- Do they have any systemic illness?
- If they have severe diarrhoea, check for additional COVID-19 infection signs.
Inquire whether the patient has ever had this issue previously, and if so, if it has been looked into. What kind of checks were made? Have there been any imaging blood tests, or endoscopies?
- Determine the patient's present line of work. Do they engage in the food or medical industries? Their managerial strategy may be impacted by this.
- Do they use alcohol or smoke?
The patient's views, worries, and expectations about the ailment and the reason it has manifested at this specific moment should be thoroughly investigated. Is the patient concerned about a particular ailment, and what do they think may be the cause?
Examination
Direct assessment
An in-person assessment should include:
- BMI and blood pressure
- Pulse rate and rhythm
- Moisture level of mucous membranes and skin
- Jaundice symptoms
- Stigmata of chronic liver disease
- Take your temperature and check your abdomen for signs of an acute abdomen
- Rectal inspection
Certain aspects of the patient's history may need additional evaluations.
Evaluation via telephone
- When evaluating someone remotely over the phone, find out:
- How do they sound? Any indication of pain?
- Can the patient feel their abdomen if they are experiencing abdominal pain? If so, is the discomfort on top of or below the umbilicus? Is it harsher when they push it or when they release it?
Video evaluation
- If evaluating through video, note:
- How do they seem; in light of their level of hydration, do their eyes appear sunken and how do they speak?
- Do they need to remain motionless if they are experiencing stomach pain? Can they evaluate rebounding or defending after receiving your instructions?
Tests
- Depending on when the symptoms started, there could be no need for examinations. Stop using any problematic drugs, then reevaluate after a suitable amount of time. If symptoms persist for more than two weeks, several simple examinations may be necessary. These may consist of blood tests such as FBC, U&Es, CRP, ESR, LFTs, TSH, HbA1c, celiac screening (tissue transglutaminase), and (if necessary) consent to HIV testing.
- Stool for culture and sensitivity, letting the lab know whether you recently travelled, went out to eat, or used antibiotics. To maximise the likelihood of finding a pathogen, it may be preferable to provide three samples on three consecutive days.
- Faecal calprotectin level, which aids in distinguishing between irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Make sure the patient hasn't taken any NSAIDs in the four weeks before. This could cause levels to be artificially raised.
- Faecal elastase in the case of suspected pancreatic insufficiency.
- Faecal immunochemical testing (FIT) may be used to help rule out lower gastrointestinal cancer. Recent NICE recommendations indicated faecal immunochemical testing as a sensitive diagnostic for ruling out lower GI cancer. When it is uncertain what may be causing a patient's lower GI problems, it should be utilised. If there is already blood on it, it should not be utilised. If used properly, a positive FIT test should trigger a two-week wait LGI referral. In primary care, this test is now easily accessible.
Referral is necessary if:
Symptoms last for more than four weeks without a primary care provider making a conclusive diagnosis:
- There is a suspicion of IBD
- Colorectal cancer
- There is a positive HIV test
- The patient needs to be admitted right away if they are critically dehydrated or are bleeding heavily
- All other tests are negative, but symptoms persist
- There is a positive FIT test
- There is a suspicion of IBD
- Raised calprotectin
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries