A guide to ophthalmic emergencies
M3 India Newsdesk Apr 12, 2022
This article provides guidance to practitioners with the presentation, examination, and management of various ophthalmic emergencies so they are able to swiftly recognise vision-threatening disorders.
Key takeaways
- It is critical to triage and evaluate the visual function and ocular integrity in patients with vision or ocular symptoms.
- The initial step is to evaluate each eye's visual acuity, preferably while the patient is wearing eyeglasses or contact lenses.
- Following that, both eyes and the surrounding periorbital tissue, including the eyelids, globes, orbits, and cheeks, are examined for obvious erythema, hematomas, lacerations, proptosis, and haemorrhage, corneal clouding, or hyphema (blood in the anterior chamber).
- Look for mydriasis, miosis, asymmetry, responsiveness to direct light, and a relative afferent pupillary deficiency in the pupils.
- This is followed by a confrontational visual field examination, evaluation of extraocular muscle (EOM) movement, slit-lamp examination (if available), and direct ophthalmoscopic fundus examination.
General and family physicians or primary care doctors are generally the first professionals to assess and diagnose any eye-related problems. Recognising and treating ophthalmic emergencies promptly may improve both systemic and ocular outcomes.
As a result, it is critical for primary care practitioners to be knowledgeable about eye-related problems. A frequent ophthalmic emergency that a physician may meet is presented, evaluated, and the following measures are discussed.
1. Eye injuries
The first evaluation of any ophthalmologic trauma is a thorough examination of the patient and attention to any potentially life-threatening injuries. Direct questions should be asked about:
- Cause and circumstances of the injury
- Any foreign body involvement
- Ocular history
- Tetanus vaccination status
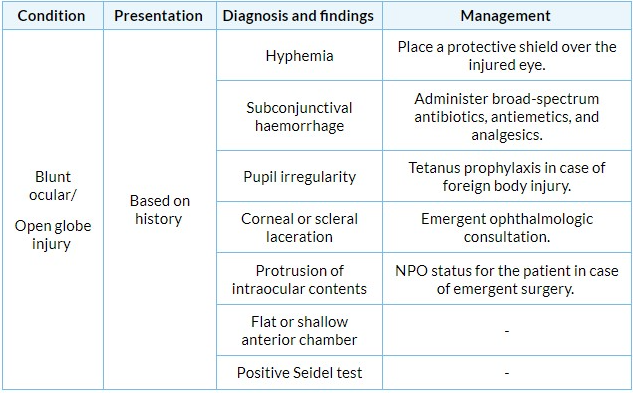
2. Blunt injury
The integrity of the cornea or sclera is compromised in an open globe injury.
Signs of injury:
- Moderate to severe pain
- Blurred vision
- Hyphema
- Pupillary distortion toward the incision
Diagnosis:
- A slit-lamp examination may reveal a reduction in the depth of the anterior chamber.
- Additionally, a Seidel test should be conducted to determine the presence of a full-thickness laceration or perforation.
- After numbing the eye with anaesthetic eye drops such as proparacaine hydrochloride 0.5 per cent, a wet fluorescein dye strip is applied to the site of damage; the eye may then be inspected with a slit lamp under cobalt-blue light.
- A positive Seidel test indicating full-thickness corneal or scleral damage would display fluorescein dye dilution surrounding the defect, as shown by a shift in the colour of fluorescein from orange to lighter yellow, and intraocular fluid flow as determined by Cobalt blue examination.
Management:
- If an open globe rupture is suspected, a protective cover should be taped over the wounded eye to prevent additional disruption of the surrounding tissue. An ophthalmologist should be contacted immediately.
- Additionally, broad-spectrum antibiotics, antiemetics, and analgesics should be provided, and the patient should be counselled to avoid eating or drinking anything by mouth in the event that urgent surgery is required.
- Prophylaxis against tetanus is also recommended if the patient's immune status is uncertain or insufficient.
- To rule out a retained intraocular foreign body, a computed tomography (CT) scan of the brain and orbits may be required.
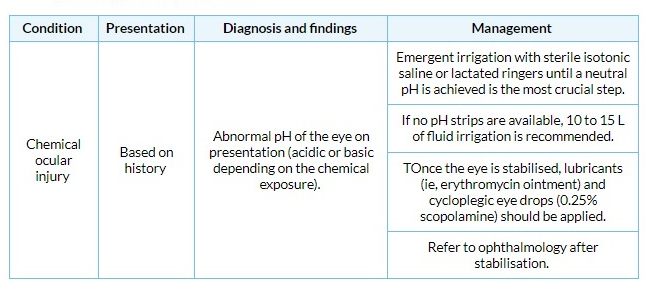
3. Chemical injury
Chemical eye injuries are often caused by:
- Spills of domestic cleaners
- Industrial chemicals
- Cement
- Automobile fluids
Diagnosis:
- The initial step in therapy should be continuous irrigation with sterile isotonic saline/lactated ringers (preferably) or tap water immediately upon presentation.
- Irrigation after a chemical splash should be undertaken before formal admission to the emergency room and prior to any additional ocular assessment or consultation with an ophthalmologist.
- If a Morgan device is available, it may be utilised to deliver ocular irrigation. To alleviate discomfort and enable irrigation, topical anaesthetic drops such as proparacaine 1% might be administered.
- By lightly touching the interior of the lower eyelid with pH indicator strips or litmus paper, determine the pH of the eye. Irrigation should be continued until a neutral pH (7.0) is obtained.
- To achieve pH neutrality, up to 10 to 15 L of fluid may be required; if litmus paper is not available, it is advised that the eye be irrigated for at least 30 minutes.
- Alkali burns are often more severe than acid burns due to their lipophilic nature, which allows them to infiltrate the eye more quickly and accumulate in tissues.
Management:
- Following proper irrigation, a thorough ophthalmologic examination should be undertaken to determine the extent of the damage.
- Lubricants on the skin, steroids, antibiotics, and cycloplegic eye drops (1 per cent cyclopentolate) are all beneficial for healing and symptom control.
- After stabilising the patient's eye, an urgent ophthalmologic referral is advised.
- Chemical burns may result in opacification of the cornea, resulting in visual impairment and chronic dry eye disease, glaucoma, and cataracts.
This is part 1 of the article. Please stay tuned for the next part in this series.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries