A Guide to Antibiotic Treatments in Adults: NICE Updates
M3 India Newsdesk Jul 07, 2023
An antibiotic prescription approach is outlined in a recently revised NICE guideline for common illnesses seen in OPD clinical practice. It seeks to maximise the usage of antibiotics while lowering antibiotic resistance.
Adult antibiotic treatments for common infections: An overview
Professionals and practitioners are obliged to thoroughly consider this directive and the unique requirements, preferences, and values of their patients or the individuals using their service while exercising their judgment.
The guidelines need to be followed with logical reasoning only, and the physician must make choices suitable for their situation after consulting with patients, their families, caretakers, or guardian.
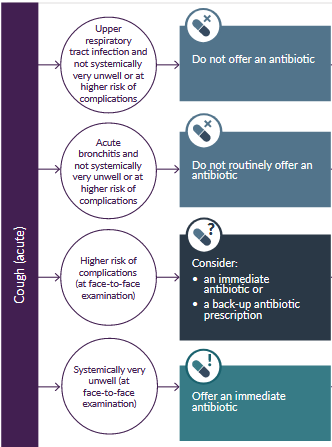
Acute cough: Antibiotic prescription
- Antibiotics have little effect on the duration of acute coughs, which are typically brought on by viral upper respiratory tract infections like the flu or cold. Acute coughs can continue for up to 3 to 4 weeks.
- Also brought on by acute bronchitis, a bacterial or viral infection of the lower respiratory tract.
- Complication risk is higher.
- People over the age of 65 who have two or more of the following conditions, or those over the age of 80 who have one or more of the following conditions:
- Prior year's hospitalisation- type 1 or type 2 diabetes
- Congestive heart failure in the past
- Present oral corticosteroid use

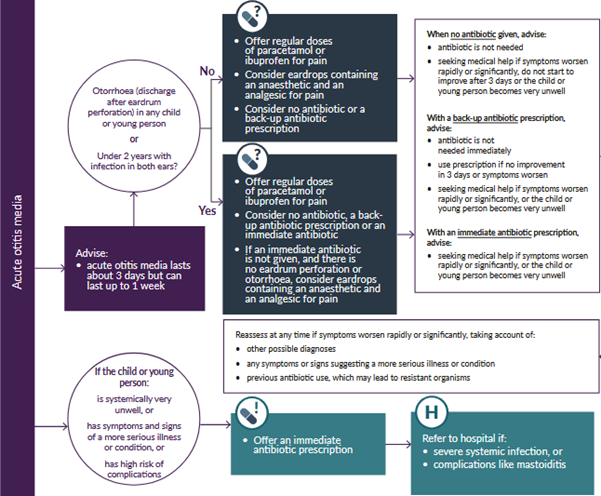
Acute otitis media: Antibiotic prescription
Non-antimicrobial therapies
Give regular doses of ibuprofen or paracetamol for pain relief. Use the highest dosages possible for severe pain and the appropriate dose for the child's age or weight at the appropriate time.
If an initial antibiotic is not administered and there is no eardrum rupture or otorrhoea, consider using eardrops that include an anaesthetic and an analgesic for pain. Evidence shows that decongestants or antihistamines do not alleviate symptoms.
Evidence about antibiotics
The percentage of children whose symptoms improve is not significantly affected by antibiotics. Antibiotics have a negligible effect on the number of kids who get recurring infections, temporary hearing loss, or eardrum perforations.
With or without antibiotics, complications (such as mastoiditis) are uncommon. Diarrhoea and nausea are potential side effects.
Those who may benefit from antibiotics more often include:
- Children under 2 years old with acute otitis media in both ears
- Children and adolescents with acute otitis media and otorrhoea (discharge after eardrum rupture)
Treatment dosage and course length
Eardrops containing an anaesthetic and an analgesic-
- Phenazone 40 mg/g with lidocaine 10 mg/g
- Apply 4 drops two or three times a day for up to 7 days
- Use only if an immediate oral antibiotic prescription is not given, and there is no eardrum perforation or otorrhoea
First-choice oral antibiotic
- Amoxicillin 1 to 11 months: 125 mg three times a day for 5 to 7 days
- 1 to 4 years: 250 mg three times a day for 5 to 7 days
- 5 to 17 years: 500 mg three times a day for 5 to 7 days
An alternative first-choice oral antibiotic for penicillin allergy or intolerance (for people who are not pregnant)
- Clarithromycin 1 month to 11 years
- Under 8 kg: 7.5 mg/kg twice a day for 5 to 7 days
- 8 to 11 kg: 62.5 mg twice a day for 5 to 7 days
- 12 to 19 kg: 125 mg twice a day for 5 to 7 days
- 20 to 29 kg: 187.5 mg twice a day for 5 to 7 days
- 30 to 40 kg: 250 mg twice a day for 5 to 7 days or 12 to 17 years: 250 mg to 500 mg twice a day for 5 to 7 days
An alternative first-choice oral antibiotic for penicillin allergy in pregnancy
- Erythromycin 8 to 17 years: 250 mg to 500 mg four times a day or 500 mg to 1,000 mg twice a day for 5 to 7 days.
- Erythromycin is preferred if a macrolide is needed in pregnancy, for example, if there is a true penicillin allergy and the benefits of antibiotic treatment outweigh.
- the harms. See the Medicines and Healthcare products Regulatory Agency (MHRA) Public Assessment Report on the safety of macrolide antibiotics in pregnancy.
Second choice oral antibiotic (worsening symptoms on the first choice taken for at least 2 to 3 days)
- Co-amoxiclav 1 to 11 months: 0.25 ml/kg of 125/31 suspension three times a day for 5 to 7 days.
- 1 to 5 years: 5 ml of 125/31 suspension three times a day or 0.25 ml/kg of 125/31 suspension three times a day for 5 to 7 days.
- 6 to 11 years: 5 ml of 250/62 suspension three times a day or 0.15 ml/kg of 250/62 suspension three times a day for 5 to 7 days.
- 12 to 17 years: 250/125 mg three times a day or 500/125 mg three times a day for 5 to 7 days.
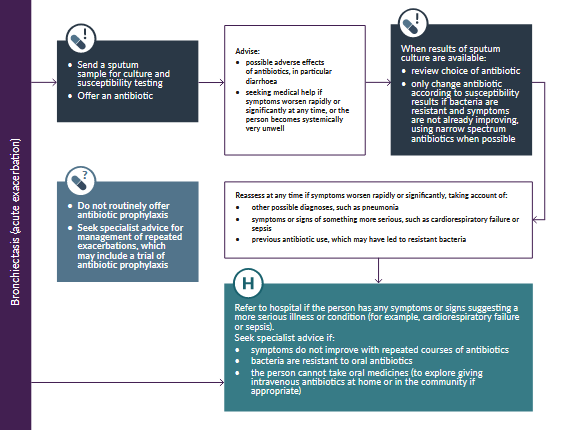
Bronchiectasis (acute exacerbation): Antimicrobial prescribing
A prolonged worsening of symptoms from a person's stable condition is referred to as an acute exacerbation of bronchiectasis.
Antibiotics - treatment
Consider the following factors when selecting an antibiotic: the severity of the symptoms; prior exacerbations, hospitalisations, and risk of complications; past sputum culture and susceptibility findings; and, if at all feasible, the use of oral antibiotics as the first line of treatment.
Antibiotics - prophylaxis
- On the guidance of a physician, only begin a trial of antibiotic prophylaxis.
- When weighing the pros and drawbacks of antibiotic prophylaxis, weigh the potential advantages (lower exacerbations), disadvantages (increasing antimicrobial resistance), side effects, and interactions with other medications, as well as the need for routine evaluation.
First choice oral antibiotics for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible)
- Amoxicillin 500 mg three times a day for 7 to 14 days
- Doxycycline 200 mg on the first day, then 100 mg once a day for a 7- to 14-day course in total
- Clarithromycin 500 mg twice a day for 7 to 14 days
Alternative choice oral antibiotics (if a person at higher risk of treatment failure) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible)
- Co-amoxiclav 500/125 mg three times a day for 7 to 14 days
- Levofloxacin (with specialist advice if co-amoxiclav cannot be used; consider
- safety issues )
- 500 mg once or twice a day for 7 to 14 days
First choice intravenous antibiotics (if unable to take oral antibiotics or severely unwell) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible).
- Co-amoxiclav 1.2 g three times a day
- Piperacillin with tazobactam 4.5 g three times a day, increased if necessary to 4.5 g four times a day.
- Levofloxacin (with specialist advice if co-amoxiclav or piperacillin with tazobactam cannot be used; consider safety issues )
- 500 mg once or twice a day
When current susceptibility data are available, choose antibiotics accordingly. Consult a local microbiologist as needed.
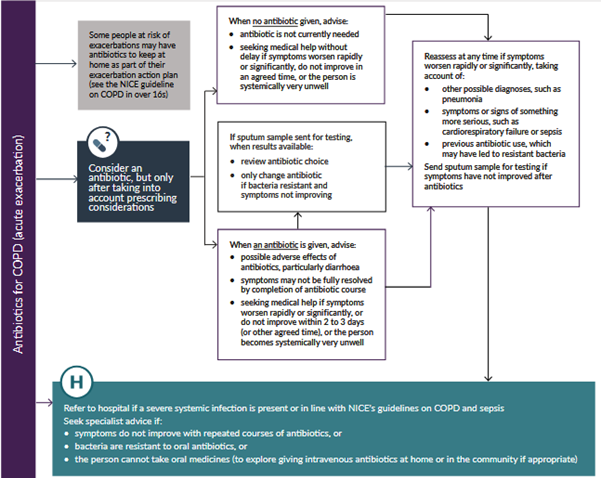
COPD (acute exacerbation): Antimicrobial prescribing
An acute exacerbation of COPD is a sustained deterioration of a person's stable symptoms.
Many exacerbations, including some severe ones, are not caused by bacterial infections and do not respond to medicines. An exacerbation may be brought on by a variety of reasons, including viral infections and smoking.
Considering prescriptions
When considering antibiotics, take the following into account.
- Whether the person may need to be treated in a hospital.
- The severity of symptoms, particularly sputum colour changes and increases in volume or thickness that go beyond the person's typical day-to-day variation.
- History of prior exacerbations and hospital admissions, as well as the risk of complications.
- The possibility of developing antibiotic resistance with repeated doses of antibiotics; past sputum culture and susceptibility findings.
- Whenever feasible, use oral antibiotics first.
Choice of antibiotic for treating an acute exacerbation: adults aged 18 years and over first choice oral antibiotics (empirical treatment or guided by most recent sputum culture and susceptibilities)
- Amoxicillin 500 mg three times a day for 5 days (see BNF for dosage in severe infections)
- Doxycycline 200 mg on the first day, then 100 mg once a day for a 5-day course in total (see BNF for dosage in severe infections)
- Clarithromycin 500 mg twice a day for 5 days
Second choice oral antibiotics (no improvement in symptoms on the first choice taken for at least 2 to 3 days; guided by susceptibilities when available)
Use an alternative first choice (from a different class) as above.
Alternative choice oral antibiotics (if the person at higher risk of treatment failure; guided by susceptibilities when available)
- Co-amoxiclav 500/125 mg three times a day for 5 days
- Co-trimoxazole4 960 mg twice a day for 5 days
- Levofloxacin (with specialist advice if co-amoxiclav or co-trimoxazole cannot be used; consider safety issues)
- 500 mg once a day for 5 days
First choice intravenous antibiotics (if unable to take oral antibiotics or severely unwell; guided by susceptibilities when available)
- Amoxicillin 500 mg three times a day (see BNF for dosage in severe infections)
- Co-amoxiclav 1.2 g three times a day
- Clarithromycin 500 mg twice a day
- Co-trimoxazole 960 mg twice a day
- Piperacillin with tazobactam 4.5 g three times a day
Consult a local microbiologist (guided by susceptibilities).
Pneumonia (community-acquired): Antimicrobial prescribing
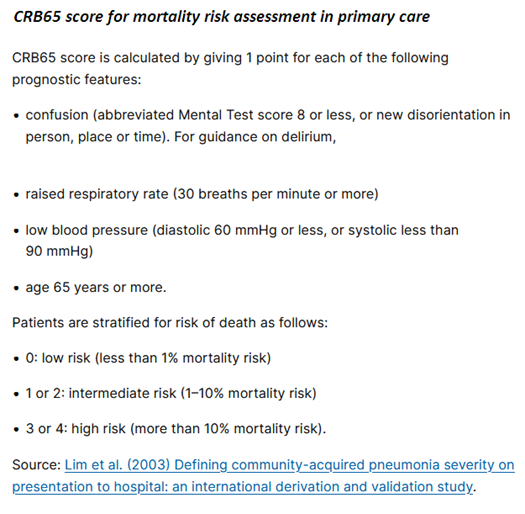
In adults, severity is assessed by clinical judgement guided by mortality risk score (CRB65 or CURB65) when calculated:
- Low severity - CRB65 score 0 or CURB65 score 0 or 1
- Moderate severity - CRB65 score 1 or 2 or CURB65 score 2
- High severity - CRB65 score 3 or 4 or CURB65 score 3 to 5
In children and young people, severity is assessed by clinical judgement.
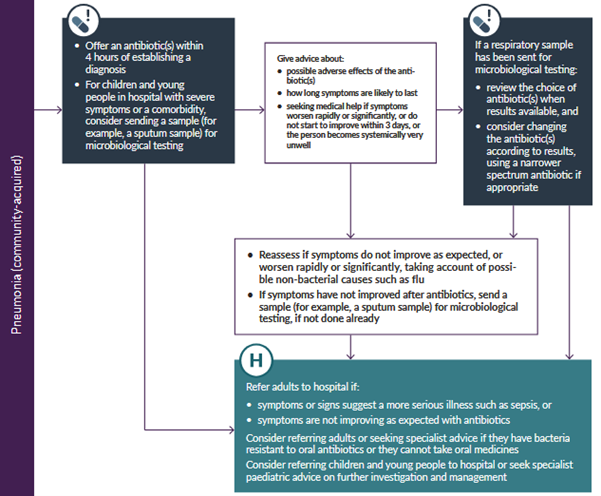
Prescribing considerations
When choosing an antibiotic(s), take account of;
- The severity assessment (adults), or the severity of symptoms or signs (children and young people).
- The risk of complications, for example, relevant comorbidity (such as severe lung disease or immunosuppression).
- Local antimicrobial resistance and surveillance data (such as flu and Mycoplasma pneumoniae infection rates).
- Recent antibiotic use.
- Previous microbiological results, including colonisation with multi-drug resistant bacteria.
Give oral antibiotics first line if possible. Review intravenous antibiotics by 48 hours and consider switching to oral antibiotics if possible.
First choice oral antibiotic if low severity (based on clinical judgement and guided by CRB65 score 0 or CURB65 score 0 or 1 when calculated). Amoxicillin 500 mg three times a day (higher doses can be used - see BNF) for 5 days.
Alternative oral antibiotics if low severity, for penicillin allergy or if amoxicillin unsuitable (for example, atypical pathogens suspected)
- Doxycycline 200 mg on the first day, then 100 mg once a day for 4 days (5-day course in total)
- Clarithromycin 500 mg twice a day for 5 days
- Erythromycin (in pregnancy)4 500 mg four times a day for 5 days
First choice oral antibiotics if moderate severity (based on clinical judgement and guided by CRB65 score 1 or 2, or CURB65 score 2 when calculated); guided by microbiological results when available
- Amoxicillin with (if atypical pathogens suspected)
- Clarithromycin or Erythromycin (in pregnancy)
- 500 mg three times a day (higher doses can be used) for 5 days
- 500 mg twice a day for 5 days
- 500 mg four times a day for 5 days
Alternative oral antibiotics if moderate severity, for penicillin allergy; guided by microbiological results when available
- Doxycycline 200 mg on the first day, then 100 mg once a day for 4 days (5-day course in total)
- Clarithromycin 500 mg twice a day for 5 days
First choice antibiotics if high severity (based on clinical judgement and guided by CRB65 score 3 or 4, or CURB65 score 3 to 5 when calculated); guided by microbiological results when available
Co-amoxiclav with:
Clarithromycin or Erythromycin (in pregnancy)
- 500/125 mg three times a day orally or 1.2 g three times a day IV7 for 5 days
- 500 mg twice a day orally or IV7 for 5 days
- 500 mg four times a day orally for 5 days
Alternative antibiotic if high severity, for penicillin allergy; guided by microbiological results when available. Levofloxacin (consider safety issues) 500 mg twice a day orally or IV for 5 days.
Consult a local microbiologist if fluoroquinolone is not appropriate.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries