7 clinical scores for pneumonia
M3 India Newsdesk Sep 21, 2021
The potential severity of pneumonia has led to the development of a number of scoring systems to understand the intensity of the disease in patients. Seven such tools have been listed in this article. The severity score derived from these tools helps clinicians to determine the required next steps in treating the patient.
CURB-65
It helps estimate the mortality of community-acquired pneumonia to help determine inpatient vs. outpatient treatment. The score is an acronym for each of the risk factors measured.
| Variable | Score |
| Confusion of new-onset | 1 |
| BUN >7 mmol/L (19 mg/dL) | 1 |
| Respiratory rate of ≥30 bpm | 1 |
| BP < 90 mmHg systolic or diastolic ≤60 mmHg | 1 |
| Age 65 or older | 1 |
- Score of 0-1 – Outpatient treatment
- Score of 2 – Admission to the medical ward
- Score of 3 or higher – Admission to intensive care unit (ICU)
Determining the score for ICU admission
The CURB-65 calculator can be used in the emergency department setting to risk stratify a patient’s community-acquired pneumonia. The percentage of mortality at 30 days associated with the various CURB-65 scores increases with higher scores.
The drastic increase in mortality between scores of 2 and 3 highlights the likely requirement for ICU admission in patients with a score of 3 or higher, as shown below:
|
CURB-65 score |
Mortality risk |
Recommendation per derivation study |
| 0 | 0.60% | Low risk, consider home treatment |
| 1 | 2.70% | Low risk, consider home treatment |
| 2 | 6.80% |
Short inpatient hospitalisation or closely supervised outpatient treatment |
| 3 | 14.00% |
Severe pneumonia; hospitalise and consider admitting to intensive care
|
| 4 or 5 | 27.80% | Severe pneumonia; hospitalise and consider admitting to intensive care |
CURB-65 is fast to compute, requires likely already-available patient information, and provides an excellent risk stratification of community-acquired pneumonia. It can facilitate better utilisation of resources and treatment initiation.
In comparison to the PSI, CURB-65 offers equal sensitivity of mortality prediction due to community-acquired pneumonia. Notably, CURB-65 (74.6%) has a higher specificity than PSI (52.2%).
SMART-COP
| 50 years old or less |
More than 50 years |
||
| Systolic BP <90 mmHg | 2 |
Systolic BP <90 mmHg |
2 |
| Multilobar CXR involvement | 1 |
Multilobar CXR involvement |
1 |
| Albumin <35 g/L | 1 | Albumin <35 g/L | 1 |
| Respiratory Rate 25 breaths/min or more | 1 | Respiratory Rate 30 breaths/min or more | 1 |
| Tachycardia 125 bpm or more | 1 |
Tachycardia 125 bpm or more |
1 |
| Confusion (acute) | 1 |
Confusion (acute) |
1 |
|
Oxygen low
|
2 |
Oxygen low
|
2 |
|
pH <7.35 |
2 | pH <7.35 | 2 |
| SMART-COP score | Risk group | Risk* |
| 0–2 | Low | Minimal |
| 3–4 | Moderate | 1 in 8 |
| 5–6 |
High Consider ICU admission |
1 in 3 |
| ≥7 |
Very high Consider ICU admission |
2 in 3 |
*Of requiring intensive respiratory or vasopressor support (IRVS)
SMART-COP is used to analyse patients with CAP who may require ICU care. CAP is the single most common cause of sepsis in older patients but can be difficult to recognise due to blunted fever and tachycardic responses to infection. It does not estimate mortality but helps stratify patients who need ICU admission.
Generally used for the population above 18 years of age with clinical and radiographic findings consistent with CAP. It does not apply to patients with significant immunosuppression.
Pneumonia Severity Index
|
Parameters |
Score |
| Age in years | |
| Male | Age |
| Female | 10 |
| Nursing home resident | 10 |
| Co-morbidity | |
| Neoplasia | 30 |
|
Liver disease |
20 |
| CKD | 10 |
| CHD | 10 |
| CVD | 10 |
| Clinical findings | |
| Altered sensorium | 20 |
| RR>30/min | 20 |
| SBO<90 % | 20 |
| Temp <35°C or >40°C | 15 |
| Pulse > 125/min | 10 |
| Investigation | |
|
pH <7.35 |
30 |
| BUN >30 | 20 |
|
Sr.Na<130 |
20 |
|
Hematocrit <30% |
10 |
|
Blood glucose > 250 |
10 |
|
PaO2< 60mmHg |
10 |
|
Pleural effusion |
10 |
| Class (score) |
Mortality rate |
Risk |
Recommendation |
| I <50 | 0.1 | Low | Treat at home |
| II 50-70 | 0.6 | Low |
Treat at home |
| III 71-90 | 0.9- 2.8 | Low | Treat at home or hospitalise |
| IV 91-130 | 8.2 -9.3 | Moderate | Hospitalise |
| V >130 |
27 – 31.1 |
High |
Consider ICU admission |
The PSI score can be used in the clinic or emergency department setting to risk stratify a patient’s community-acquired pneumonia. Its purpose is to classify the type of severity of a patient’s type of CAP and allocate medical management and determine the number of resources to be utilised for care. Most commonly, the scoring system has been used to decide whether patients with pneumonia can be treated as outpatients or as inpatients (hospitalised).
It provides an excellent risk stratification of CAP. However, for most patients with clinically diagnosed CAP, the CURB-65 is easier to use and requires fewer inputs to calculate.
SOAR criteria
| Parameters | Value | Score |
|
Systolic BP Or Diastolic BP |
<90 mmHg <60 mmHg |
1 |
|
Oxygenation, PaO2/FiO2 |
<250 | 1 |
| Age | ≥ 60 years | 1 |
|
Respiratory rate |
≥ 30/min | 1 |
| SOAR Score | Management | 30-day mortality |
| 0-1 | OP | <8% |
| >2 | IP | 33% |
It is a modified version of CURB-65, where it excludes “confusion” & “BUN” and adds “PaO2” criteria. Usually used for patients with radiologically or clinically diagnosed pneumonia in a nursing home and helps dispose them as outpatient or inpatient management. The SOAR score also provides 30-day mortality depending on their type of management, that is – outpatient or inpatient (hospitalised).
SOAR is also a superior alternative for better identification of severe nursing home-acquired pneumonia (NHAP).
ATS/IDSA criteria for severe CAP
Severe CAP is defined as the presence of one major criterion or at least three minor criteria.
|
Minor criteria |
| Respiratory rate ≥30 breaths per min |
| Partial pressure of oxygen/fraction of inspired oxygen ratio [PaO2/FIO2 ratio] ≤250 |
| Multilobar infiltrates |
| Confusion/disorientation |
|
Uremia (BUN level ≥20 mg per dL) |
|
White blood cell count <4,000 per μL due to infection alone (i.e., not chemotherapy-induced) |
|
Thrombocytopenia (platelet count <100,000 cells per mm3) |
|
Hypothermia - core temperature < 96.8ºF (36ºC) |
|
Hypotension requiring aggressive fluid resuscitation |
|
Major criteria |
| Respiratory failure requiring mechanical ventilation |
|
Severe shock requiring vasopressors |
The Pneumonia Severity Index (PSI) is recommended to determine the need for hospitalisation, whereas the ATS/IDSA criteria for severe CAP are recommended to predict the need for intensive care. Routine treatment of CAP with macrolide monotherapy is no longer recommended unless local resistance is low. Amoxicillin and doxycycline are preferred in low-risk patients. Five-day treatment courses are recommended for all patients with CAP, with reassessment following treatment.
The minor criteria were superior to other prognostic scoring systems (including the PSI, CURB-65 score, and SCAP) for predicting the need for mechanical ventilation, vasopressor support, and ICU admission.
| Variable | Points | |
| Arterial pH <7.30 | Yes | 13 |
| No | 0 | |
| Systolic pressure <90 mmHg | Yes | 11 |
| No | 0 | |
| Respiratory rate >30 breaths/min | Yes | 9 |
| No | 0 | |
| BUN >30 mg/dL (>10.7 mmol/L) | Yes | 5 |
| No | 0 | |
|
Altered mental status (e.g. confusion) |
Yes | 5 |
| No | 0 | |
| PaO2 <54 mmHg (or PaO2/FiO2 <250 mmHg) | Yes | 6 |
| No | 0 | |
|
Age ≥80 years |
Yes | 5 |
| No | 0 | |
|
Multilobar/bilateral X-ray |
Yes | 5 |
| No | 0 |
Severe Community-Acquired Pneumonia (SCAP) Score
| SCAP score* |
Risk of SCAP** |
| 0 | 0.27-3.43% |
| 1-9 |
0.66-3.25% |
|
10-19 |
9.23-11.24% |
|
20-29 |
36.62-41.82% |
|
≥30 |
50% |
*Patients with scores ≥10 are classified as having severe community-acquired pneumonia and are recommended for ICU, monitored bed, and/or immediate intervention.
**Defined as in-hospital death, septic shock, and/or need for mechanical ventilation.
In the emergency department, after diagnosis of community-acquired pneumonia is made, calculating SCAP may help predict the chance for “severe CAP”, defined by adverse outcomes including inpatient mortality, septic shock and/or need for mechanical ventilation. It assists with disposition decisions after diagnosing CAP in the emergency department. A high-risk SCAP showed higher rates of adverse outcomes than high-risk PSI and CURB-65, potentially helping choose which patients are at most need for the ICY with higher specificity.
Clinical Pulmonary infection (CPIS)
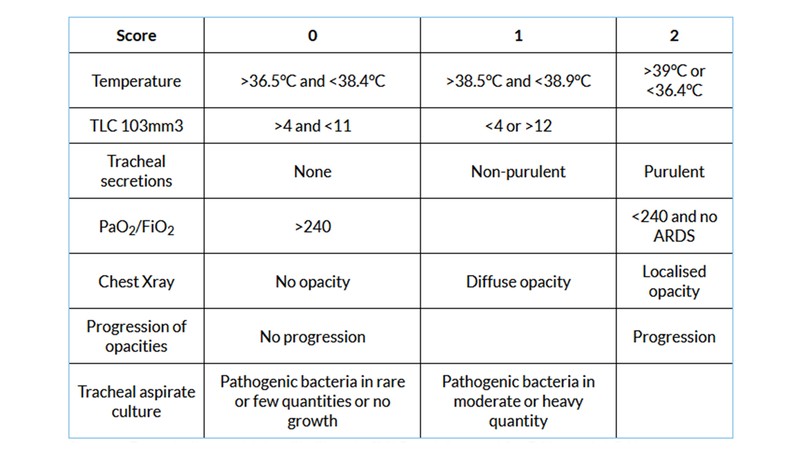
Scores ≥ 7 may indicate a higher likelihood of VAP and the need for BAL or mini-BAL.
It assists in diagnosing ventilator-associated pneumonia (VAP) by predicting the benefit of pulmonary (sputum or bronchial-alveolar lavage) cultures. CPIS is utilised in patients being evaluated for potential ventilator-associated pneumonia.
A CPIS value ≥7 reproducibly allowed to differentiate ventilator-associated tracheobronchitis (VAT) from ventilator-associated pneumonia (VAP) with high specificity. The CPIS has been most successfully used in guiding treatment decisions for patients with a low likelihood of VAP, for whom CPIS-guided therapy has resulted in lower costs and reduced development of antimicrobial resistance.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries