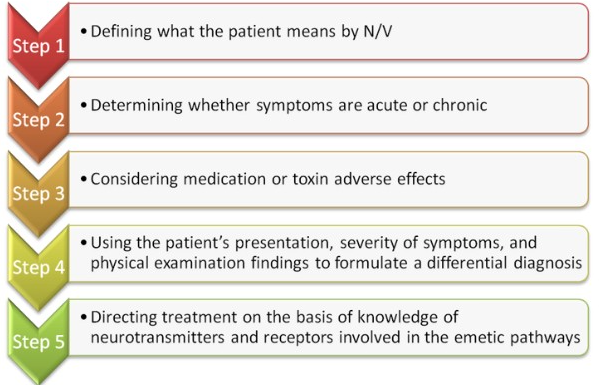
5-step strategy in managing nausea and vomiting
M3 India Newsdesk Apr 22, 2022
Clinical management of nausea and vomiting may be complicated, given the large variety of probable underlying causes and diagnostic and therapeutic alternatives. This article discusses the clinical management of nausea and vomiting (N/V) by using a 5-step strategy.
Kay takeaways
- Vomiting and nausea are multifactorial symptoms.
- Utilising a logical five-step method may assist in narrowing the vast differential diagnosis and directing therapy.
- A thorough history and physical examination provide the diagnostic foundation for N/V assessment and guide diagnostic tests.
- Antiemetic and prokinetic medicines are used to treat the underlying condition and alleviate symptoms. In patients with persistent, resistant symptoms, complementary and alternative therapy may be investigated.
Treatment of acute or mild symptoms may entail an empirical trial of antiemetics without comprehensive testing. When symptoms are persistent or moderate-severe, testing for an underlying cause should be conducted, with a particular emphasis on pharmaceutical side effects, neurologic reasons, gastrointestinal illnesses, metabolic or endocrine abnormalities, and psychogenic disorders.
In outpatient and inpatient settings, N/V are typical presenting ailments. These symptoms have been linked to an increased risk of morbidity and a worse quality of life, especially in individuals with chronic problems. Doctors who work in both primary care and subspecialty settings can use this short review to learn how to evaluate and treat N/V. The five-step approach entails:
Step 1
Defining what the patient means by N/V
It is crucial to distinguish N/V from other symptoms such as retching, regurgitation, and rumination.
- Nausea is a subjective sense of an upset stomach or throat that often precedes vomiting.
- Vomiting is a very specialised bodily occurrence characterised by the quick and forceful oral evacuation of stomach contents followed by an abdominal muscle spasm.
- Retching is an aggressive and recurrent spasmodic contraction of the abdominal muscle with the glottis closed but no stomach contents being expelled.
- Regurgitation, on the other hand, is the passive retrograde passage of oesophagal or gastric contents back into the mouth without the typical diaphragmatic or muscular activity associated with vomiting. Regurgitation is a defining feature of gastroesophageal reflux disease.
- Rumination is a deliberate rise in abdominal pressure that results in the regurgitation of partly digested food back into the mouth. Regurgitation often alleviates stomach discomfort or pressure in persons with rumination.
Patients may misunderstand the symptoms of regurgitation and rumination as N/V; so, the first step is to differentiate vomiting from regurgitation and rumination, since their diagnosis and therapy are radically different.
Step 2
Determining whether symptoms are acute or chronic.
- In contrast to chronic N/V, which is characterised by symptom length of four weeks or more, acute N/V is defined by symptom duration of seven or fewer days.
- The majority of instances of acute N/V are caused by a temporary medical disease (e.g., viral gastroenteritis), a self-limited somatic problem (e.g., musculoskeletal trauma; acute myocardial infarction), or a brief drug side effect.
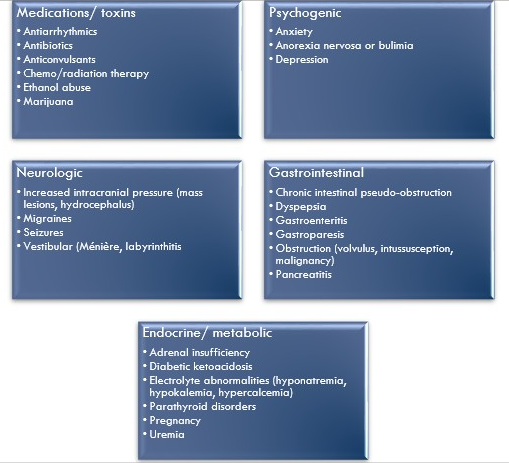
- As a result, acute N/V is often treated symptomatically without doing a thorough cause review. It is often beneficial to explore the following key etiologic groups when dealing with chronic N/V: drug adverse effects, neurologic reasons, gastrointestinal ailments, metabolic and endocrine abnormalities, and psychogenic disorders.
Step 3
Considering medication or toxin adverse effects.
- Medication reactions are a frequent cause of N/V, particularly during the first few days following treatment commencement, although the development of symptoms may be subtle.
- Numerous medicines have been implicated in the development of N/V; typical offenders include nonsteroidal anti-inflammatory drugs, antiarrhythmic agents, antibiotics, antiepileptic drugs, opiates, and levodopa.
- Medications and poisons most likely cause N/V by activating the CTZ situated in the region postrema of the fourth ventricle's ventral side.
- Furthermore, chemotherapy and radiation treatment are also well-established causes of N/V. Female sex, younger age, concomitant anxiety, and past history of nausea and vomiting (N/V) are all risk factors for chemotherapy-induced nausea and vomiting (CINV).
- Another critical factor to consider is postoperative N/V. Symptoms often manifest 24 hours after surgery and may be induced by anaesthetics, opioids, or other adverse medication responses.
Neurologic
- Numerous neurologic diseases may result in N/V. A wide range of conditions, including central nervous system mass lesions, infection and hydrocephalus, may cause vomiting with or without nausea if the intracranial pressure rises, such as idiopathic intracranial hypertension. Ménière illness, vestibular schwannoma, and benign paroxysmal positional vertigo are all labyrinthine causes of N/V.
- The N/V of motion sickness is induced by recurrent vestibular nuclei activation. Additionally, N/V is usually connected with migraine headaches and seizures. N/V may be associated with both acute and chronic pain.
Gastrointestinal
- Gastrointestinal irritants induce enteroendocrine cells of the intestinal epithelium to produce serotonin (5-HT3), which triggers 5-HT3 receptors on afferent vagal nerves.
- This activation is the primary mechanism that initiates the vomiting reflex after consumption of noxious chemicals or when the gastrointestinal mucosa is ulcerated, inflamed, or distended.
- The many gastrointestinal illnesses that result in N/V may be classified as acute or chronic. Acute symptoms may occur as a consequence of infections (for example, gastroenteritis), inflammatory illnesses (for example, pancreatitis or appendicitis), or intestinal blockage (eg, volvulus, intussusception, or strangulated hernia).
- Chronic N/V may be caused by a variety of conditions, including dyspepsia, gastroparesis, and chronic intestinal pseudo-obstruction.
Endocrine and Metabolic
- By activating the CTZ in the region postrema, metabolic and endocrine disturbances induce afferent input into the vomiting centre. Numerous metabolic and endocrine illnesses, such as diabetic ketoacidosis, uremia, adrenal insufficiency, hyperparathyroidism, and thyroid abnormalities, may result in N/V.
- Pregnancy is the most prevalent endocrine cause of N/V, affecting up to 50%–75% of women, although hyperemesis gravidarum affects just 1%–5% of pregnancies and is treated with pyridoxine (vitamin B6).
- N/V may also display electrolyte problems such as hyponatremia, hypokalemia, and hypercalcemia. Paraneoplastic syndromes and hematologic diseases, especially acute intermittent porphyria, are less prevalent causes.
Psychologically induced
Numerous mental disorders may be linked to N/V as a result of emotional or physical stresses. Anxiety, sadness, anorexia nervosa, and bulimia nervosa are examples of these illnesses.
Step 4
Develop a differential diagnosis based on the patient's presentation, the severity of symptoms, and physical examination results and lead the further investigation with laboratory, imaging, and procedural testing.
The patient's medical history
- The history provides the diagnostic foundation for assessing N/V. It is critical to get specific information on the start of symptoms (rapid vs gradual), the timing (in relation to eating, frequency), the kind of emesis (undigested or partly digested food, presence of bile, volume), and related symptoms (abdominal pain, weight loss, early satiety, bloating, change in bowel habits, and neurologic deficits).
- Vomitus description, time of vomiting, and related symptoms are often useful in eliciting a diagnosis (Refer to the table above). A thorough examination of the patient's comorbid conditions, prescription list, and history of drug abuse (e.g., alcohol, cigarettes, marijuana) should be conducted.
Physical examination
- Dehydration symptoms (skin turgor and mucous membranes) and evaluation of orthostatic vital signs should be the emphasis of the physical examination, particularly in the inpatient environment.
- t is important to observe the existence of lymphadenopathy, jaundice, abdominal tumours, and indications of despair and anxiety. Systemic characteristics such as increased skin and mucosal hyperpigmentation in Addison disease, tremor or lid lag in thyrotoxicosis, and lanugo with calluses on the dorsum of the hands in self-induced vomiting may all give critical diagnostic information.
- The abdominal examination is critical because it may assist limit the diagnosis further by revealing signs such as a succussion splash, which indicates stomach outlet blockage. A cranial nerve and neurologic examination may be necessary in people presenting with neurologic and vestibular complaints.
- Vestibular dysfunction has been documented in up to 26% of individuals who originally presented to a gastroenterologist with chronic N/V.
Laboratory testing
- A full blood count and electrolyte analysis are performed at the first laboratory exam. Additional laboratory tests should be ordered mostly on the basis of the patient's history and physical examination.
- Pregnancy tests for women of childbearing age, inflammatory markers (C-reactive protein) for a suspected inflammatory process, serum drug levels or urine drug screen for ingestion concerns, pancreatic or hepatic enzyme activities for gastrointestinal processes and glycosylated haemoglobin levels in diabetic patients are examples.
- Additional laboratory tests to consider include the thyroid-stimulating hormone level (hypothyroidism), morning cortisol level (adrenal insufficiency), and blood calcium concentration (hypercalcemia).
Additional imaging and tests
- The history, physical examination, and laboratory testing should all be used to guide the first diagnostic diagnosis. For patients with moderate N/V without warning symptoms, antiemetic medication may be started without further imaging.
- Abdominal radiography may be the initial diagnostic imaging test of choice for patients with suspected gastrointestinal aetiology. In certain circumstances, abdominal computed tomography cross-sectional imaging may be indicated.
- When structural or anatomical reasons for dysphagia are ruled out, esophagoduodenoscopy or oesophagal manometry may be investigated. A gastric emptying study may be done on individuals with suspected gastroparesis.
- Brain magnetic resonance imaging may be the next step in people with suspected central nervous system causes.
- After a thorough history, physical examination, and diagnostic evaluation have been completed and confirmed to be unremarkable, persons with persistent, unexplained N/V might seek a psychogenic assessment.
Step 5
Directing treatment on the basis of knowledge of neurotransmitters and receptors an involved in the emetic pathways
Treatment and care
When possible, the initial step in treating patients is to discontinue potential problematic drugs. This is especially critical when there is a temporal relationship between the initiation of medication and the onset of symptoms. Additionally, dietary change may be undertaken, with careful attention to oral intake and nutritional support. Once a definite diagnosis of N/V is made, therapy is focused on the underlying illness.
Pharmacological treatments
- After adequate fluid and electrolyte replenishment, a range of antiemetic and prokinetic medications may be employed to treat N/V. While several medicines are effective in managing acute N/V, persistent symptoms may be more difficult to control. The fifth step is to guide therapy based on an understanding of the neurotransmitters and receptors involved in central and peripheral emetic pathways.
- The 5-HT3 antagonists exert their action by centrally inhibiting the CTZ and peripherally inhibiting intestine vagal afferents. They are extremely successful in treating N/V due to the stimulation of both central and peripheral pathways caused by the widespread expression of 5-HT3 receptors.
- QT interval prolongation is critical to consider, especially in patients with arrhythmias and those taking several QT-prolonging medications simultaneously.
- Phenothiazines (e.g., prochlorperazine, promethazine) and butyrophenones (e.g., droperidol, haloperidol) inhibit D2 dopaminergic receptors and are beneficial in patients with centrally induced vomiting, such as migraine headaches, motion sickness, and vomiting associated with hazardous drugs.
- Extrapyramidal side effects are a worry; the risk varies according to the patient's age and drug dosage and has been reported to be as high as 25%.
- The second-generation neuroleptic olanzapine is an intriguing option because to its excellent antinausea and antiemetic activity and decreased likelihood of extrapyramidal side effects.
- Anticholinergic and antihistamine drugs (e.g., diphenhydramine, meclizine) work on the central anticholinergic (M1 receptor) and antihistamine (H1 receptor) systems, respectively. They are especially effective in treating N/V associated with vertigo and motion sickness due to their action on the vestibular system and CTZ.
- However, care should be used while using these medicines in the elderly, since they have been known to cause disorientation, urine retention, visual abnormalities, and constipation. Metoclopramide is an antiemetic medication with prokinetic characteristics that is beneficial in the treatment of gastroparesis. It works by inhibiting vagal and cerebral 5-HT3 and D2 receptors. Long-term usage is constrained by the possibility of permanent extrapyramidal side effects (akathisia, parkinsonism, and tardive dyskinesia).
- Neurokinin 1 receptor antagonists act by reducing substance P's emetic effects and have been licenced by the Food and Drug Administration for the treatment of CINV.
- Cyclic vomiting syndrome, for example, might be very difficult to manage. Patient education and counselling are critical components of the interdisciplinary care of N/V functional and psychogenic diseases.
- Functional N/V may be treated with medications such as olanzapine and mirtazapine, with mirtazapine boosting appetite and improving sleep in some individuals.
- Additionally, pain treatment is critical, since abdominal discomfort is a common symptom in persons with chronic N/V. Opioids should be avoided since they have been shown to impair stomach motility and cause nausea.
Additional Therapies
Surgery is recommended for some types of N/V. (eg, gastric outlet obstruction). Enteral feeding by percutaneous endoscopic gastrostomy or jejunostomy may be explored for patients with severe, refractory symptoms or diseases that do not respond to surgical resection (eg, metastatic malignant disease). Enteral nutrition is preferable over parenteral nourishment wherever feasible.
Additionally, a number of integrative and alternative treatments for chronic N/V have been described, including acupuncture, hypnosis, and herbal supplements such as ginger and pyridoxine. Nonetheless, these medicines often have insufficient evidence based on research with small sample numbers and uneven effects. Cannabinoids have been licenced for the treatment of CINV, but their long-term usage may result in CHS. Cannabinoids, in general, should not be used frequently to treat N/V.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries