Case discussions on common issues in newborns: Dr. Balaji Chinnasami & Dr. Janani Arul
M3 India Newsdesk Mar 16, 2020
Dr. Balaji Chinnasami and Dr. Janani Arul, in this series, provide assistance to general practitioners in treating patients by providing them with ready-made evidence-based prescriptions.

Young infant with fever
A 45-day-old full term infant weighing 4.2 kg, presents with fever over a 1-day duration. The baby is on exclusive breastfeed, feeding well and thriving well. Physical examination shows no localising signs, temperature 100ºF, normal cry, normal fontanel, and no organomegaly.
Science behind management
- There is a high risk of serious bacterial infection in young infants (<3 months) with fever.
- Inconsolable crying, drowsiness, abnormal respiration, poor peripheral circulation, petechiae, seizures are red flags for serious illness.
- Less than one month old babies or sick-looking babies with fever should be hospitalised for parenteral antibiotics.
- Infants with no signs of serious illness and available for close follow up can be managed on outpatient basis with oral antibiotics.
Investigations to run
- Complete blood count with differential (5000 to 15000 per mm3 is normal)
- C-reactive protein (>2 mg/dl or >19 nmol per L is abnormal)
- Blood culture whenever feasible
- Urine analysis (pyuria or bacteriuria) and urine culture
- Chest X-ray if there are any respiratory findings
- Stool routine and culture if diarrhoea is present
- Lumbar puncture for infants <1 month (may be omitted for older infants)
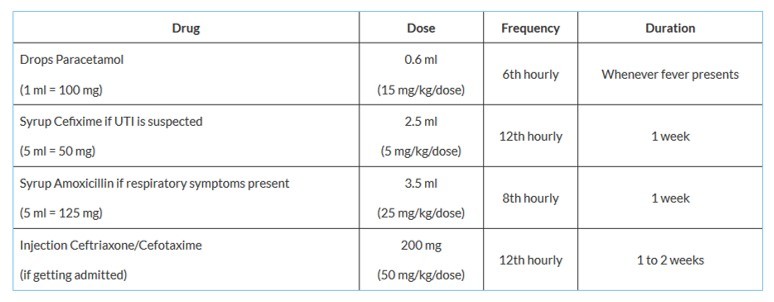
Rx
Advice to give to parents
- Continue breastfeeding the baby on demand.
- Danger signs like poor feeding, lethargy, convulsions, vomiting, cold peripheries, abnormal breathing warrant immediate return to hospital.
- Temperature should be monitored.
Poor weight gain in a newborn
A 2-week-old newborn with birth weight of 3.1 kg presents with a current weight of 2.8 kg. There were no issues at birth. The baby was delivered via C-section and discharged on the third day. The mother reported that though she has good secretion of breast milk the baby was not sucking at the breast well.
Science behind management
- Newborns lose weight during the initial 3 to 4 days of life. Following the initial weight loss, they are expected to gain 30 to 40 g/day on an average.
- Cumulative weight loss >10% of birth weight/failure to gain birth weight in 2 to 3 weeks is usually due to inadequate feeding.
- The most common cause of inadequate feeding is ineffective suckling or inadequate breast milk supply.
- Supplementary feeding with infant formula can cause weight gain but often results in cessation of breastfeeding.
Breastfeeding assessment
Directly observe breastfeeding session with a trained nurse/doctor. Make sure that the baby’s mouth is wide open and sucks at both nipple and areola. Nipple sucking is the main cause of sore nipple and poor milk transfer to the baby.
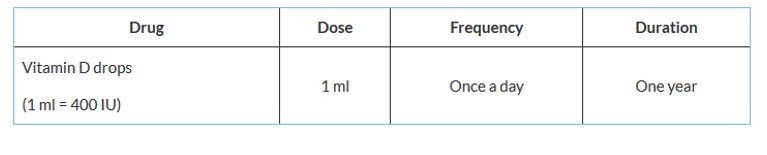
Rx
Advice to give to parents
- Follow immunisation as per schedule.
- Follow up within a week to check for weight gain.
- Revisit immediately if danger signs like inability to feed, vomiting, convulsions, or lethargy present.
- If there is concern of decreased milk supply, express breast milk manually/using breast pump and give it as spoon feeds. Breast milk expression stimulates the breasts to secrete more milk.
- If the infant is already on formula, feed the infant each time with any available breastmilk before giving formula and avoid bottle feeding.
- Suggest videos available online like on Youtube on breastfeeding attachment, expression of milk for training.
Care plan for preterm babies (<37 weeks)
A 10-day-old, preterm (35 weeks) baby with 2.1 kg birth weight following a normal neonatal transition is brought for routine follow up care. Physical examination reveals normothermic condition, stable vitals, and pink, not icteric skin. Systemic examination is normal.
Science behind management
- Routine blood investigations and oral vitamin supplementation are required to prevent anaemia and osteopenia of prematurity.
- Regular neurodevelopmental assessment can pick up developmental delays at an early stage.
- Use special growth charts like Fenton chart to track weight, height and head circumference. Roughly babies grow 15 to 20 g/kg/day.
- Premature babies should be put on exclusive breastfeeding. If sucking is less effective, the mother should be advised to express breastmilk and give it in addition to direct breastfeeding.
- For infants with subnormal weight gain (<15 to 20 g/kg/day), breastmilk can be fortified with nutrients such as human milk fortifier (one HMF sachet 2 g in 50 ml of milk).
Blood investigations to run
- Complete blood count with peripheral smear
- Thyroid profile
- Calcium, alkaline phosphatase and phosphorous (Osteopenia of prematurity)
- Serum bilirubin
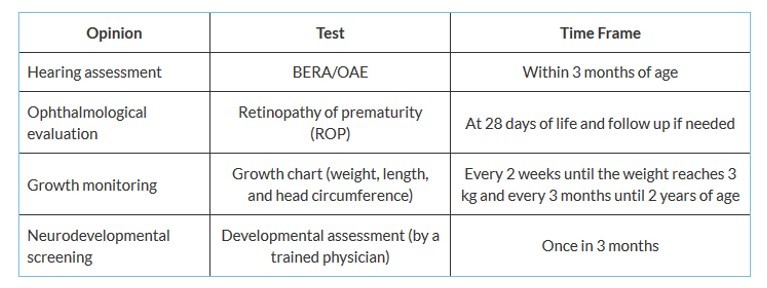
Screening of preterm babies
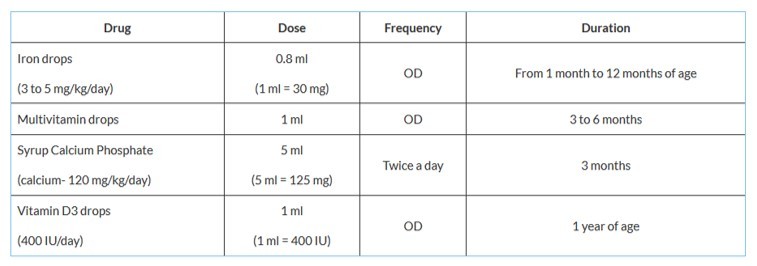
Rx
Advice to give to parents
- Routine immunisation should be done as per chronological age. Also Influenza vaccine should be administered at 6 months of age.
- Kangaroo Mother Care (KMC) should be practiced at least twice a day.
- Breastfeed on demand as it is essential for weight gain.
Neonatal hyperbilirubinemia
A 6-day-old full term, male baby with birth weight of 3.4 kg was brought by the mother with complaints of yellowish discolouration of the eyes. The baby was on direct breast feeds. The mother’s blood group (MBG) was A positive and the baby’s blood group (BBG) was O positive.
Science behind management
- Jaundice appears first in the face and then progresses to the trunk and then palms and soles as the severity of jaundice increases. Jaundice should not be assessed by conjunctival icterus in neonates.
- Weight loss and inadequate feeding is the most important cause of hyperbilirubinemia.
- Any jaundice persisting for more than 14 days is persistent jaundice and needs further evaluation.
- Cholestatic jaundice (direct bilirubin high, clay coloured stools and high coloured urine) requires urgent evaluation to diagnose surgically treatable conditions like biliary atresia.
- Scalp swellings (cephalhematoma/sub-galeal haemorrhage) should be a part of routine.
Investigations to run
- Serum total and direct bilirubin in case of ABO incompatibility (mother blood group is O and baby blood group is either A or B) and Rh incompatibility (MBG is Rh negative and BBG is Rh positive)
- Complete blood count with peripheral smear, reticulocyte count, Direct Coombs Test (DCT)
Treatment
- Phototherapy (as per bilirubin normogram) 20 mg/dl from fourth day of life is the rough cut off for starting phototherapy.
- Cholestatic jaundice- Plan for immediate evaluation and surgery if needed.
Advice to give to parents
- Continue breastfeeding on demand.
- Do not expose newborns to direct sunlight because they might get sun-burned.
Click here for recommendations on further reading
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
Dr. Balaji Chinnasami is a Professor of Paediatrics and Medicine at a reputed medical college in Chennai.
Dr. Janani Arul is an Assistant Professor of Paediatrics from Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries