New checkpoint inhibitor shows promise in clinical trial for non-Hodgkin's lymphoma: NEJM
Newswise Nov 08, 2018
By combining the experimental anticancer antibody known as 5F9 (Hu5F9-G4) with the established anticancer antibody rituximab, researchers managing a small phase 1b clinical trial were able to induce a positive response in 11 out of 22 people with relapsed/refractory non-Hodgkin’s lymphoma.
About 36% of the patients (8 out of 22) in this trial went into complete remission from their cancers. This new approach to immunotherapy, published November 1, 2018 in the New England Journal of Medicine, relies on immune system cells called macrophages, rather than T cells, to attack and kill cancer cells.
“5F9 is a macrophage immune checkpoint inhibitor,” said Sonali Smith, MD, the Elwood V. Jensen Professor in Medicine, Director of the Lymphoma Program at the University of Chicago Medicine, and senior author of the study. “This is one of the first successful anticancer drugs that can stimulate a macrophage to attack a cancer cell. It opens a whole new door.”
The cell surface marker CD47, displayed by many cancer cells, is a “don’t ‘eat me’ signal,” Smith explained. Macrophages don’t normally attack those cells. But there is a second “eat me” signal that is potentiated by the other antibody, rituximab. The combination of 5F9 and rituximab “can overcome the signals that protect these cancer cells,” she said.
“This is incredibly exciting,” she added. Checkpoint inhibitors “don’t work very well in non-Hodgkin’s lymphomas,” she explained. “Now we may have a way to manipulate the immune system for people with non-Hodgkin’s lymphomas that have relapsed and progressed after multiple prior therapies. And we can do it with limited side effects.”
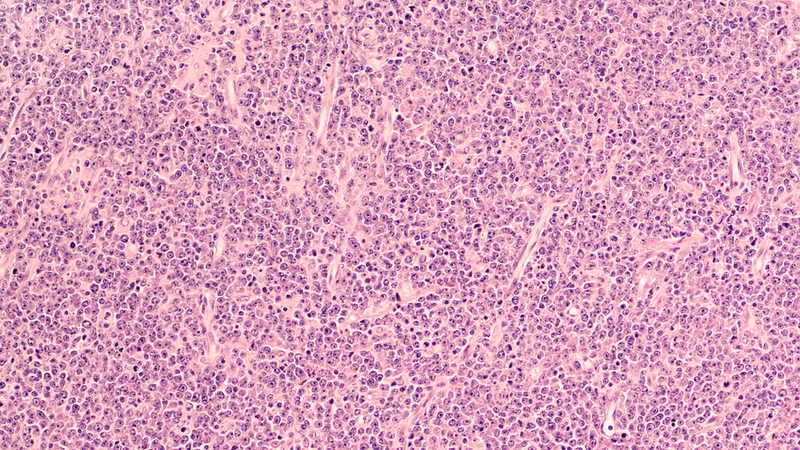
All 22 patients in the study had failed to respond to, or relapsed after, at least 2 and as many as 10 previous types of therapy. Fifteen patients had diffuse large B-cell lymphoma (DLBCL) and seven had follicular lymphoma. “Keep in mind,” Smith said, that “diffuse large B-cell lymphoma, when it progresses after second-line treatment, is usually a fatal disease.”
All patients were treated with a combination of 5F9 at slowly increasing dosages and rituximab. Treatment, on average, lasted 22 weeks. Eleven patients showed a clinically significant reduction in their cancers. In eight of those patients, all signs of cancer were eliminated. The other three patients died due to disease progression.
Forty percent of patients in the DLBCL subgroup achieved objective response and 33% reached a complete response. Seventy-one percent of patients in the follicular lymphoma subgroup had an objective response and 43% achieved complete response.
The first full remission in the trial was a University of Chicago Medicine patient. She had relapsed within 3 months of an autologous stem cell transplant, was wheelchair bound, with rapidly progressive, very aggressive lymphoma. Within a week after starting therapy, “she began to feel better,” said Smith. “By the first assessment, after 4 weeks of treatment, she was in a complete remission.”
The study authors report there were “no unacceptable side effects, and the maximum tolerated dose was not reached.” The treatment can cause low-grade anemia that resolves. Patients did not see the adverse side effects often seen in T-cell checkpoint inhibitors, such as nivolumab or pembrolizumab, although the numbers of patients treated so far is small.
Patients who had a prior CAR T-cell therapy, however, did not respond to this treatment. “There may be something about CAR-T that exhausts the T cells,” Smith suggested. “This is not a T cell-mediated approach, but there appears to be some effects on the immune system that may make it less likely to work in this setting.” The researchers have agreed to exclude people who have a disease recurrence after CAR T-cell therapy.
This approach to treatment began almost a decade ago. In 2010, researchers led by Irving Weissman, MD, director of the Stanford Institute for Stem Cell Biology and Regenerative Medicine, showed that nearly all cancer cells coat themselves with the protective “don’t eat me” protein known as CD47. Weissman and colleagues subsequently developed the antibody they called Hu5F9-G4 that blocks the CD47 protein, enabling macrophages to engulf and devour these unmasked cancer cells.
Much of the underlying biology was elucidated by Mark Chao, MD, PhD, a former graduate student in the Weissman laboratory who performed a series of essential studies in mice leading to the first clinical studies of Hu5F9-G4. The summary for a 2010 paper in the journal Cell noted that “Treatment of human NHL-engrafted mice with anti-CD47 antibody reduced lymphoma burden and improved survival, while combination treatment with rituximab led to elimination of lymphoma and cure.”
In an editorial about the study in the NEJM, the authors—Alberto Mantovani, MD, (University of Milan) and Dan L. Longo, MD, (Queen Mary University of London)—conclude that “if confirmed and extended” the results could “pave the way to macrophage checkpoint blockade as a new immunotherapy strategy.”
—Newswise
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries