What do you know about CREST syndrome?
M3 India Newsdesk Jan 04, 2022
The treatment of CREST syndrome remains a significant challenge despite the advances made in understanding its key pathogenic events. Recently, with the understanding of immune alterations behind the syndrome and the developments of targeted immune therapies, there has been an improvement in the prognosis of the disease. This article presents a brief about all the clinical features and the treatment protocols currently in place.
What is CREST syndrome?
CREST syndrome (Calcinosis, Raynaud phenomenon, Esophageal dysmotility, Sclerodactyly, and Telangiectasia) is a member of the heterogeneous group of sclerodermas, and its name is an acronym for the cardinal clinical features of the syndrome.
Systemic scleroderma (SSc) is a multisystem disease with microvascular abnormalities, autoimmune disorders, excessive collagen production and deposition, fibrosis of the skin and internal organs, with the progressive course and potentially fatal outcomes. SSc is a multisystem connective tissue disease of an unknown aetiology that affects the skin and is certainly associated with genetic factors, immune system alterations, and environmental factors.
The Committee of the American Academy of Dermatology proposed a comprehensive classification of cutaneous sclerosis in three large groups:
- Primary cutaneous sclerosis
- Diffuse systemic or limited systemic (CREST syndrome)
- Localised or circumscribed without the involvement of internal organs
- Secondary cutaneous sclerosis as a result of GVHD (Graft versus Host disease), intoxication, infections, use of medications.
- Prodromal cutaneous sclerosis syndromes, primarily Raynaud’s phenomenon.
Pathophysiology
The pathogenesis of the disease involves:
- Vascular abnormalities that result in tissue hypoxia.
- Immune responses manifested with altered T- and B-lymphocyte functions.
- Production of autoantibodies, through fibroblast dysfunction and excessive collagen synthesis.
Genetic factors clearly influence disease susceptibility. HLA (human leukocyte antigen) genes have been implicated in the susceptibility to SSc. T cell-derived cytokines initiate damage of the blood vessels and indirectly cause tissue hypoxia; they also directly stimulate fibroblasts to increase collagen synthesis.
Elevated serum interleukin-2 levels, activated lymphocytes in the biopsy specimens, activated monocytes in the peripheral blood, reduced number of CD8+ T lymphocytes, impaired function of NK (natural killer) cells, presence of various autoantibodies and immune complexes, all prove the immune system alterations associated with SSc.
Endothelial cells are among the first targets. Precapillar sphincter dilation causes microvascular hypertension, swelling, telangiectasia, and later arteriolar hyperplasia and fibrosis. Excessive collagen production results in fibrosis of the skin and internal organs, collagen (types I, III, IV, and VII), fibronectin, glycosaminoglycans, and proteoglycans are deposited in the interstitium and in the intima of small arteries.
Calcinosis
Calcinosis is one of the typical manifestations of CREST syndrome. It is associated with problems of poor peripheral circulation, causing local skin irritation, inflammation, ulceration that encourages secondary infection.
Calcinosis generally results from dystrophic calcification associated with massive collagen degeneration. Dystrophic calcification is due to the accumulation of calcium apatite crystals, with normal levels of serum calcium, phosphorus, and alkaline phosphatase.
Calcium deposits develop in the skin, as subcutaneous nodules or massive nodes, mainly in the elbows, knees, fingers and toes, but also in other body areas.
Raynaud's phenomenon
Raynaud’s phenomenon (RPh) causes numbness, pain and colour changes in fingers. It is triggered by exposure to cold or emotional stress. Due to the spasm of small blood vessels (capillaries) one or more fingers suddenly turn white, become cold and insensitive.
After a few minutes or longer, lack of oxygen in the blood causes cyanosis and pain in the fingers, but when the circulation gets normal, hyperemia occurs and the skin gets red. Secondary RPh is typical for collagen and vascular diseases.
It is usually asymmetric and may be accompanied by ulceration or necrosis. Primary RPh affects younger individuals, after stressful events or exposure to cold; changes are symmetrical without ulcerations and necrosis.
Oesophageal dysmotility
The earliest abnormality in the involved gut of scleroderma patients is dysmotility secondary to nerve injury, perhaps resulting from arteriolar changes in the vasa nervorum or compressive nerve damage via collagen deposits. Smooth muscle atrophy occurs later (and often marks the beginning of symptoms).
The predilection for smooth muscle rather than striated muscle atrophy explains the distribution of anatomic involvement. The proximal oesophagus primarily is a striated muscle and remains essentially uninvolved. The oesophagus typically is weakly responsive to prokinetic therapy, until the final stage of the disease (fibrotic infiltration of muscle) halts the response to medications.
The consequences of oesophagal dysmotility are reflux and its complications. The reduced LES pressure in patients with scleroderma likely allows acid reflux, which is exacerbated by delayed clearance of acid from the oesophagus because of abnormal distal motility. This creates an environment in which stricture, Barrett oesophagus, adenocarcinoma, or aspirations may occur.
Oesophageal dysmotility is usually found in the lower two-thirds of the oesophagus and the lower oesophagal sphincter, due to smooth muscle atrophy and fibrosis of the lamina propria and submucosa, atrophy and mucosal erosion and disruption of the capillary network. Patients often state they must drink liquids to swallow solid food. Oesophagal reflux is common, as well as nausea, vomiting, weight loss, diarrhoea, constipation and bleeding.
Sclerodactyly
The development of sclerodactyly begins with a perivascular inflammatory infiltrate in the dermis. The trigger for this inflammatory process is not known. It is the thickening that generally only involves the skin of the fingers (and toes) distal to the metacarpophalangeal joints in CREST syndrome. Sclerodactyly evolves through three phases:
- Edematous phase- Begins with finger swelling, morning stiffness, and arthralgias.
- Indurative phase- The skin becomes thickened, shiny, without wrinkles, erythematous, and itchy.
- Atrophic phase- The skin becomes fragile and lax, although it looks thicker due to tight connections with the structures underneath.
The fingertips are pointed, fixed in an acutely flexed position, with ulcerations and calcifications. The distal phalanges are shortened or missing. Hands are stiffened into a claw and become immovable. The nails are dystrophic, dry, striated and deformed. Skin distal to the elbows and knees, neck and face may be observed.
Telangiectasias
Telangiectasias can be seen in SSc due to dilatation of capillaries, and are common on the hands, face, mucosal surfaces, and sometimes on the trunk. Telangiectasias blanch on applying pressure. They can increase over time and are considered to be associated with an increased risk of pulmonary hypertension.
Laboratory studies
- ANAs: Limited scleroderma is associated with an early rise in ANA levels.
- Anti centromere antibodies: These are found in approximately 50-90% of patients with limited forms of scleroderma. These antibodies are present in 82-96% of patients with the CREST variant.
- Calcinosis: Evaluate serum calcium and phosphorus levels to exclude a metabolic disturbance; however, calcinosis resulting from limited scleroderma is not associated with calcium or phosphorus abnormalities.
- Raynaud phenomenon: The presence of ANA predicts the development of connective-tissue disease.
- Oesophageal dysmotility: Patients who are positive for ANAs and anticentromere antibodies while also being negative for anti-Scl70 antibodies appear to have more oesophagal involvement.
- Sclerodactyly: A thyrotropin level may help exclude the presence of thyroid disease as another potential cause of edematous or thickened skin.
- Telangiectasia: No laboratory data are necessary.
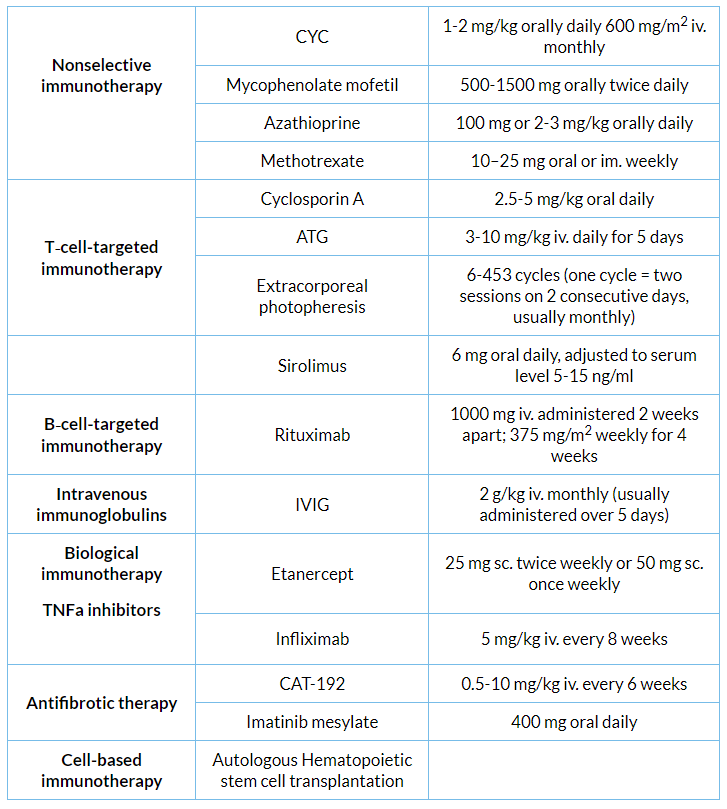
Immunotherapeutic treatment in systemic sclerosis
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries