Well-appearing febrile child: How to diagnose & treat?: New AAP guidance
M3 India Newsdesk Dec 06, 2021
Well appearing febrile infants if not properly evaluated and treated, are at risk of missing serious bacterial infections like meningitis, bacteremia and urinary tract infection. In this article, we present a brief tabulated summary of the new American Academy of Paediatrics (AAP) guideline and a few case scenarios to better understand the key action statements.
The 38-page clinical practice guideline by AAP attempts to develop an evidence-based approach to manage febrile infants.
Major questions addressed were:
i) What investigations are to be done?
ii) Who should be admitted?
iii) Should we do a lumbar puncture for all?
iv) Should we give parenteral or oral antibiotics?
v) When can antibiotics be stopped and the patient discharged?
Practice pearls
- In a well-looking, 8-21 day old, febrile neonate, after taking lumbar puncture, blood culture, and urinalysis/urine c/s the patient should be admitted and started on parenteral antibiotics until cultures come sterile.
- In a well-looking, 22-28 days old febrile neonate lumbar puncture is optional if inflammatory markers are negative. The patient should be admitted and treated with parenteral antibiotics if CSF or urinalysis is abnormal. If all investigations are normal, the infant may be managed at home after giving parenteral antibiotics and reassessed in 24 hours.
- In a well-looking, 29-60 days old febrile infant admit for parenteral antibiotics if CSF analysis is abnormal. The patient can be managed at home with oral antibiotics if UTI is suspected, and with no antibiotics, if all investigations are normal.
Summary of management of well-appearing febrile infants
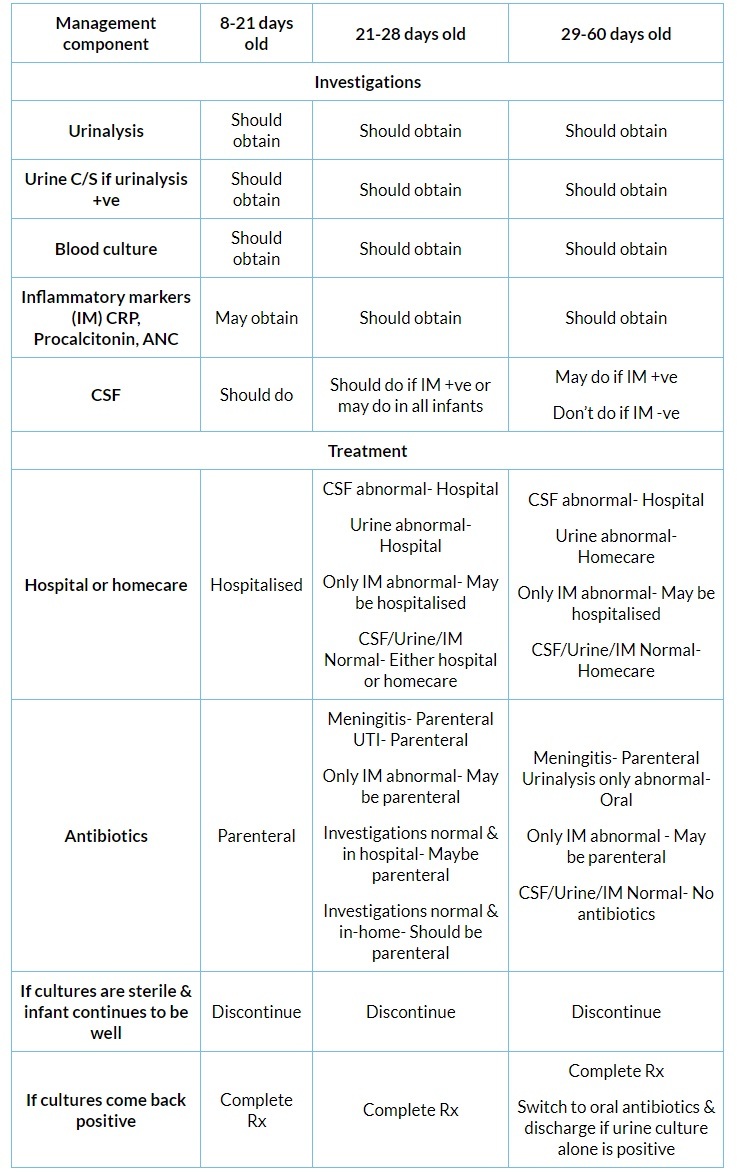
CSF analysis includes WBC, protein, glucose, gram stain and culture for bacteria.
Notes:
- Urinalysis consists of a urine culture specimen obtained by suprapubic aspiration/catheterisation.
- Infants monitored at home should be reassessed in the following 24 hours.
- IMs are considered abnormal if temperature >38.5°C, procalcitonin >0.5 ng/ml, CRP >20 mg/L and Absolute Neutrophil Count (ANC) >4000-5200 per mm3.
- HSV should be considered in infants with vesicles, seizures, mucus membrane ulcers, leukopenia, thrombocytopenia and CSF pleocytosis with the absence of positive gram stain. Add acyclovir in such cases.
Case 1
A ten-day-old, well-appearing, normally breastfeeding neonate presented with fever and had no obvious source of infection.
Investigations done:
- Blood culture
- Lumbar puncture for CSF analysis
- Urinalysis- 5 pus cells/ HPF, leukocyte esterase was positive. Since urinalysis was suggestive of UTI, urine culture by suprapubic aspiration/catheterisation was done.
- CRP- 6 mg/dl, Procalcitonin- was not done; Absolute Neutrophil Count (ANC) was 5000/mm3.
Practice notes: Inflammatory markers like CRP are not compulsory as we will admit and treat with antibiotics irrespective of their values.
Treatment followed: The baby was admitted to the hospital and started on parenteral antibiotics (Inj. Ceftriaxone 250 mg IV BD*).
Progress of the case: All cultures came back sterile and the neonate continued to be well. We discontinued antibiotics and discharged the patient after 24 to 36 hours.
Case 2
A twenty-five days old, well-appearing infant presented with fever. The infant was feeding well with no obvious cause for fever.
Investigations done:
- Blood culture
- Urinalysis- Leukocyte esterase positive
- Inflammatory markers- CRP- 1 mg/dl & negative, Procalcitonin- 2 ng/ml & positive, ANC- 7000/mm3 & positive
Next sequence of investigations:
- Since urinalysis was positive, urine culture was done by suprapubic aspiration/catheterisation.
- Since inflammatory markers, procalcitonin & ANC were abnormal, lumbar puncture was done.
- Cells - 20 leukocytes/mm3 (>5 leukocytes/mm3 is pleocytosis)
- Protein- 45 mg/dl (Normal)
- Glucose- >2/3rd of blood sugar (normal)
Practice notes:
- CSF analysis may be done in all 21-28 days old febrile infants, but definitely should be done if inflammatory markers are abnormal.
- If inflammatory markers are abnormal but CSF and urinalysis are normal, the infant may be admitted and parenteral antibiotics given till culture reports.
- If all investigations are normal, the infant may be managed at home after giving parenteral antibiotics and reviewing after 24 hours.
Treatment done: In view of CSF pleocytosis/urinalysis being positive, the infant was admitted to the hospital and parenteral antibiotics were started (Inj. Ceftriaxone 250 mg IV BD).
Progress of the case: Blood culture showed growth. CSF culture, urine culture showed no growth. Hence, antibiotics should be continued to complete the full course. If cultures are negative and the child is stable, antibiotics can be discontinued.
Case 3
A fifty-day-old, well-appearing infant presented with fever, no cough, and no other source of infection.
Investigations done:
- Blood culture
- Urinalysis- No pus cells, leukocyte esterase was negative
- Inflammatory markers- CRP & procalcitonin were elevated, ANC was within range
Follow up investigations:
- Since urinalysis was negative, no urine culture was required.
- Since inflammatory markers were positive, a lumbar puncture was performed.
- CSF- cells- no pleocytosis
- Proteins and sugar- Normal
Treatment done:
Since CSF analysis was negative, oral antibiotics were tried. (Syr. Cefixime 50 mg 2.5ml twice a day was started).
Practice notes:
- If CSF analysis is positive, the patient should be admitted and administered parenteral antibiotics.
- If urinalysis/inflammatory markers are positive, manage at home with oral antibiotics.
- If all investigations are normal, manage at home without antibiotics.
Progress of the case: All cultures were sterile. Hence oral antibiotics were discontinued.
*Choice of antibiotic not mentioned by AAP
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Balaji Chinnaswami is a professor of Paediatrics at a reputed medical college in Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries