Vitamin D Toxicity: Symptoms, Diagnosis and Treatment
M3 India Newsdesk Apr 09, 2024
This article delves into vitamin D toxicity's various facets, including its symptoms, risk factors, diagnostic criteria, treatment approaches, long-term effects, and pertinent case studies.
Vitamin D
In addition to being synthesised in the human body by sun exposure, vitamin D is a fat-soluble vitamin that can be found in certain animal food sources. Further, vitamin D is sold as an over-the-counter supplement and under prescription. Known as the "sunshine vitamin," vitamin D is essential to many physiological functions in the human body.
Vitamin D is widely known for its critical role in bone health, but it also affects cardiovascular health, immunological function, and mood control. Even while vitamin D is necessary, high doses can be harmful and pose serious health hazards.
Role of vitamin D and its requirements
Vitamin D plays a crucial role in maintaining calcium and phosphorus balance which is essential for healthy skeletal development and appropriate bone mineralisation. Moreover, it supports neuromuscular function, controls cellular growth, and modifies immunological responses.
For most people, adequate amounts of vitamin D are ensured by dietary intake and sunshine exposure. But some groups—older people, people who don't get much light, people with malabsorption disorders—might need to take supplements. Age-specific recommendations vary, with adults generally consuming between 600 and 800 international units (IU) per day.
Aetiology
- Taken intentionally or unintentionally, excessive vitamin D intake can cause vitamin D toxicity in healthy adults.
- Toxicological consequences might potentially arise from prescription errors without regular monitoring of vitamin D levels.
- Patients who require large dosages of medication to address conditions such as osteoporosis, renal osteodystrophy, psoriasis, gastric bypass surgery, celiac disease, or inflammatory bowel disease are often at risk of toxicity due to inadequate monitoring.Toxic effects have resulted from fortifying foods or supplements with higher than recommended levels of vitamin D.
- Glades Drugs' multivitamins were voluntarily recalled by the FDA in 2015 because of high vitamin D content. The Danish Health Authority recalled a supplement in 2016 due to vitamin D levels that were 75 times greater than advised. At least twenty kids experienced development.
- Fish, meat, and dairy items all contain vitamin D, though rarely in amounts high enough to be toxic.
- Individuals who take large dosages of vitamin D and unintentionally consume more highly fortified milk are also more vulnerable to vitamin D poisoning. It may also arise from overproduction of 1,25(OH)2D in diseases such as lymphomas and granulomatous illnesses.
- Because of how vitamin D is regulated and transformed into inactive metabolites, excessive sun exposure does not result in vitamin D toxicity.
- Vitamin D toxicity has also been linked to rodenticide exposure that contains cholecalciferol, despite the majority of cases being observed in animals.
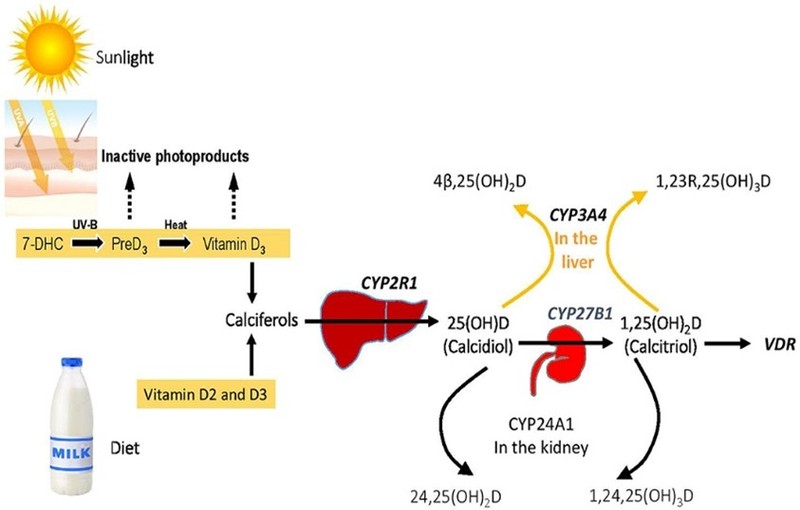
Pathophysiology
Adipose tissue and the liver both store fat-soluble vitamin D. It can be obtained from external sources and is produced internally by the human body.
According to the Endocrine Society's clinical practice guidelines, persons between the ages of 19 and 50 should consume 600 IU/d of vitamin D daily. The daily need for those between the ages of 50 and 70 is 600 IU/d. The recommended daily intake for individuals over 70 is 800 IU/d. The highest recommended daily intake for individuals over the age of eight is 4000 IU/d.
Vitamin D is metabolically inactive and requires a series of metabolic transformations to become its active form. This includes forms acquired from external sources or through endogenous synthesis.
The skin naturally transforms provitamin D3 (7-dehydrocholesterol) into vitamin D3 (cholecalciferol). UVB light acts as a catalyst for this process. Vitamin D-binding protein (VDBP) in the serum carries vitamin D3, which is obtained from food and sun exposure. The enzyme vitamin D-25-hydroxylase then transforms vitamin D3 into 25-hydroxyvitamin D3 [25(OH)D] in the liver. Following creation, VDBP carries 25(OH)D to the kidneys. It is changed into calcitriol, or 1,25-dihydroxy vitamin D3, in the proximal convoluted tubules by 25(OH)D-1-α-hydroxylase [1,25(OH)2D]. Once within the body, 1,25(OH)2D is mostly used to control calcium metabolism. It is subsequently delivered to other parts of the body by VDBP. Vitamin D stimulates osteoclast activity, which is crucial for the resorption of calcium from bone.
Vitamin D is stored primarily in the liver. The liver has a negative feedback regulation of the vitamin D-25-hydroxylase enzyme, but it is insufficient to stop toxicity.
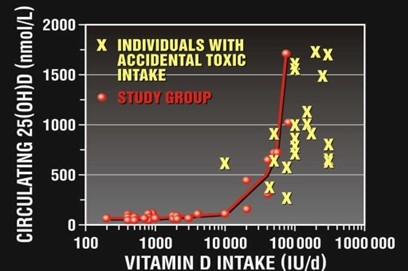
High vitamin D intake causes the liver and adipose tissue to store the nutrients, which saturates the receptors that bind to vitamin D. This raises the levels of 25(OH)D and many other vitamin D metabolites.
Vitamin D metabolites, such as 25(OH)D, 24,25(OH)2D, 25,26(OH)2D, and 25(OH)D-26,23-lactone, have much higher amounts when there is hypervitaminosis D. The VDBP-binding capacity is exceeded by abnormally high quantities of vitamin D metabolites, which releases free 1,25(OH)2D. Although this theory hasn't been confirmed beyond a reasonable doubt, higher quantities of free 1,25(OH)2D and 25(OH)D are thought to be the cause of vitamin D toxicity.
Symptoms and clinical manifestations
- Vitamin D poisoning can present with a wide range of symptoms, from vague signs to severe ones.
- Weakness, exhaustion, nausea, and vomiting are some of the early symptoms.
- People may suffer from symptoms like disorientation, frequent urination, constipation, and dehydration as the poisoning worsens.
- Calcium stones and other renal issues, such as bone pain, may develop from vitamin D toxicity.
- Severe cases may result in potentially fatal consequences such as kidney damage, hypercalcemia, and cardiovascular problems.
Risk factors
Vitamin D intoxication develops as a result of multiple circumstances. One of the main causes is excessive supplementing, which frequently results from incorrect prescriptions or ignorant self-administration. Furthermore, a number of illnesses, including granulomatous disorders and hyperparathyroidism, increase the risk of vitamin D poisoning.
There are intrinsic hazards associated with long-term UV radiation exposure and eating foods fortified with high levels of vitamin D.
Diagnostic criteria and laboratory tests
Vitamin D toxicity diagnosis requires a thorough review that includes laboratory tests, clinical assessment, and patient history. The foundation for diagnosis is serum 25(OH)D levels; amounts greater than 150 ng/mL are suggestive of toxicity. Assessing blood parathyroid hormone, calcium, and phosphorus levels concurrently helps to define the degree of dysregulation and related problems.
Treatment approaches
The basic principles of managing vitamin D intoxication are stopping supplements and treating underlying causes. In moderate situations, blood levels can be returned to normal by stopping vitamin D intake and drinking enough water.
Severe toxicity warrants aggressive measures, including intravenous fluids, diuretics, and corticosteroids to mitigate hypercalcemia and alleviate associated symptoms. In select instances, haemodialysis may be warranted to expedite the clearance of excess vitamin D metabolites.
Clinical management of vitamin D toxicity is mainly supportive and focuses on lowering calcium levels. Vitamin D and calcium supplements should be discontinued. In addition, excessive bed rest should be avoided to prevent hypercalcemia due to immobilisation.
Isotonic saline should be used to correct dehydration and increase renal calcium clearance. In severe toxicity resulting in severe hypercalcemia (serum calcium >14 gm/dL), calcitonin and bisphosphonates can be used. Dosing is recommended as follows:
- Up to 48 hours of injectable calcitonin at a dose of 4 U/kg can be given once every 12 hours.
- The intravenous bisphosphonates zoledronic acid (4 mg IV over 15 minutes) and napidronate (90 mg IV over 2 hours) can be given together.
- It has been demonstrated that the coadministration of bisphosphonates with calcitonin increases the former's effectiveness.
- Tachyphylaxis may result from calcitonin, however the effects of bisphosphonates may last longer. Thus, when taking these drugs, calcium levels need to be closely watched.
- Although it is debatable, intravenous glucocorticoids are typically used to treat vitamin D toxicity associated with granulomatous illness. The way this drug acts is by lowering plasma calcium levels via decreasing calcitriol levels.
- It assists by lowering intestine absorption and raising calcium excretion in the urine.
- Prednisone 40 mg/d or hydrocortisone 100 mg/d for five days.
- Patients may require hemodialysis to treat refractory hypercalcemia or renal failure.
- To modify the dosage of vitamin D supplements in the future, the patient's medication list should be examined.
- To prevent overusing vitamin supplements, patients must receive counselling.
The Endocrine Society suggests monitoring 25-hydroxy vitamin D and calcium serum levels for patients on high-dose vitamin D replacement therapy.
Differential diagnosis
Vitamin D hypervitaminosis should be differentiated from other causes leading to hypercalcemia. Other diseases that mimic the signs and symptoms of hypervitaminosis are as follows:
- Hypercalcemia of malignancy
- Hypercalcemia of granulomatous diseases
- Primary, secondary, and tertiary hyperparathyroidism
- Vitamin A toxicity
- Thyrotoxicosis
- Paget disease
- Hypercalcemia caused by prolonged immobilisation
- Milk-alkali syndrome
Long-term effects and complications
- Acute symptoms of vitamin D toxicity usually go away with timely treatment, but long-term exposure to high vitamin D levels might cause long-term problems.
- Individuals with persistent hypercalcemia are at risk for cardiovascular consequences, nephrolithiasis, and renal impairment.
- Osteoskeletal demineralisation and soft tissue calcification are long-term effects that require close observation and treatment.
Case studies
Case of Hypervitaminosis presenting a renal calculus
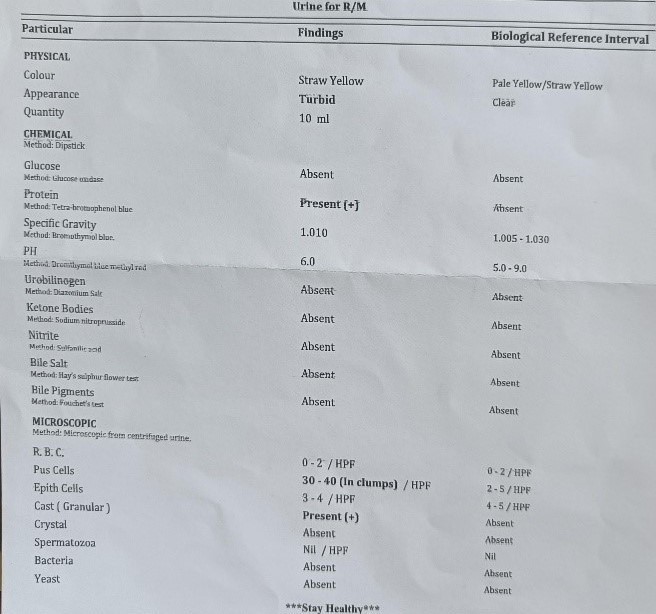
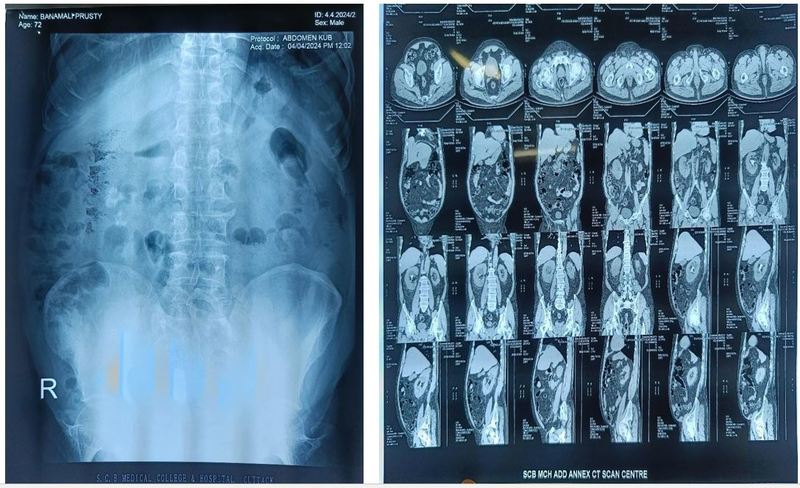
A 72-year-old diabetic male presented with fever for 5 days, with burning micturition and pain in the lower abdomen associated with urgency and hesitancy. On examination of urine, it showed pus cells, USG showed bilateral renal Calculi, and x-ray KUB also showed the same on metabolic evaluation serum calcium was raised, se vit D3 level was 200 ng/mL. on retrograde questioning, the patient was found to have a history of long-term intake of calcium+ D3 tablets.
Take-home message
- Vitamin D toxicity is a complex clinical entity with a range of symptoms, diagnostic difficulties, and treatment issues.
- Optimising patient safety and reducing the risk of toxicity need careful observation, wise supplementation, and clinician knowledge.
- By cultivating a sophisticated comprehension of vitamin D metabolism and toxicity dynamics, medical professionals may effectively navigate this clinical terrain and protect their patients' well-being.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
Co-author: Dr Saswati Satpathy is an MD Biochemistry, Senior Resident.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries