Vertigo: Classification and clinical challenges in the management: Dr. Aneesh Basheer
M3 India Newsdesk Jun 06, 2022
This article gives a broad classification of the challenging condition of vertigo and its clinical management, which could help clinicians while dealing with such patients.
Key takeaways
- Vertigo may not always be described as a spinning sensation by patients.
- Temporal profile, aggravating factors, history of antecedent risk factors and associated symptoms may help differentiate central from peripheral lesions causing vertigo.
- Nystagmus is a useful sign to distinguish central from peripheral causes; central lesions may be associated with direction-changing nystagmus with a gaze.
- HINTS examination is a simple method to determine the likelihood of a central cause.
- MRI with MRA is the preferred imaging when the central lesion is suspected.
- The threshold for ordering imaging must be low in older age, risk factors for stroke, focal neurological deficits and persistent symptoms beyond 48 hours.
The vertigo conundrum
This common symptom may be perceived as spinning, swaying or illusion of movement despite the classic definition of sense of rotation. The rotation may be of the self or of the environment. Some patients may find it difficult to exactly describe the symptom and use the vague and nonspecific term dizziness.
The latter term also includes presyncope, disequilibrium and ill-defined lightheadedness. Further, vertigo is not a diagnosis; rather it is a symptom that needs detailed evaluation.
For the clinician, vertigo is a challenge since it may indicate underlying conditions as benign as benign paroxysmal positional vertigo (BPPV) to ominous ones like an acoustic neuroma. The broad classification of vertigo into peripheral and central helps narrow down differentials based on history and clinical examination (table 1).
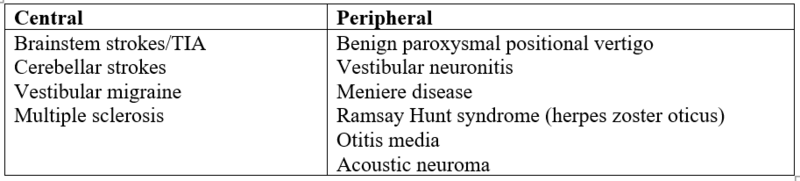
Table 1. Common causes of peripheral and central vertigo
Clinical characteristics of vertigo
Features that may help indicate peripheral or central causes include:
- Prominent nystagmus out of proportion to vertigo is more likely to be central.
- Severe vertigo is more likely to be peripheral.
- Severe nausea and vomiting are highly suggestive of peripheral vertigo.
- Gait and postural stability are more likely to be disturbed in central vertigo.
- Drop attacks characterized by a sudden loss of tone resulting in falling without any loss of consciousness is often a feature of advanced peripheral vertigo such as Meniere disease (Tumarkin’s crisis).
Diagnosis
A systematic historical approach is critical to making a diagnosis.
1. Temporal profile- The temporal profile is very useful as evident from some examples below:
- Very short duration (less than 1 minute) - usually seen in BPPV
- Several minutes to hours - migraine or posterior circulation TIA
- Hours - Meniere disease
- Days - vestibular neuronitis, multiple sclerosis, brainstem or cerebellar stroke
Single episodes are more in favour of migraine while most other conditions cause recurrent episodes of vertigo.
2. Aggravating factors- Aggravating factors may sometimes help in identifying the cause.
- Cough, sneeze or loud sounds may aggravate vertigo due to perilymphatic fistula.
- It must also be noted that aggravation of vertigo with head movements may occur in all types of vertigo and cannot be used to narrow down the differential diagnosis.
3. Potentially provoking factors- Potentially provoking factors need to be elicited through history such as:
- Recent head trauma (may predispose to perilymphatic fistula and BPPV)
- Recent middle ear surgery (may suggest perilymphatic fistula)
- Viral prodrome or fever preceding symptoms (acute vestibular neuronitis)
- Severe hyperextension injury to the neck (brainstem stroke due to vertebral artery dissection)
- Recent use of drugs like aminoglycosides or phenytoin
4. Other symptoms- Enquiring about other symptoms may be a useful exercise as:
- History of cranial nerve dysfunction (diplopia or dysphagia) and/or other focal deficits may indicate brainstem stroke.
- Tinnitus and hearing loss may be indicative of Meniere's disease.
- Progressive hearing loss and features of raised intracranial tension and/or involvement of trigeminal nerve may suggest acoustic neuroma.
- Headache with aura, photophobia or phonophobia must raise suspicion of migraine.
The clinical examination must be targeted to identify signs that enable distinguishing central from peripheral causes (Table 2).

Table 2. Clinical findings that may be useful in vertigo
5. Nystagmus- Nystagmus is an important sign and has to be evaluated carefully. In peripheral lesions, the fast component is towards the normal ear. Further, it increases in amplitude and frequency on looking towards the normal ear.
Fixation of vision tends to reduce or suppress nystagmus in peripheral lesions. Moreover, nystagmus due to peripheral lesions never changes direction even when the direction of gaze is changed, unlike central lesions where it may reverse.
6. HINTS- HINTS refers to head impulse, nystagmus and skew deviation. The presence of any one of the three HINTS components namely a normal head impulse, direction-changing nystagmus and skew deviation is supposed to predict central vertigo.
Role of imaging
Most patients will not require specialised tests based on a good history and examination. If preliminary enquiry suggests a central lesion or acoustic neuroma, MRI brain is the investigation of choice. When a vascular lesion is suspected, it is often prudent to order an MR angiogram as well. The decision to perform imaging must be based on the possibility of a central lesion, older age, persistent symptoms and/or risk factors for stroke.
Audiometry and brainstem auditory evoked potentials may be useful in assessing hearing loss. Other less commonly ordered (and less useful) tests are the electronystagmography, video-nystagmography and magnetic evoked potentials.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author, Dr Aneesh Basheer is an Academician Professor of Medicine from Kerala. He is an expert reviewer of international peer-reviewed medical journals and case reports.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries